Statins in Chronic Obstructive Pulmonary Disease (COPD): A Feasibility Study to Control Frequent Exacerbations Needing Hospitalization in Kashmiri Population
Received Date: January 06, 2022 Accepted Date: February 06, 2022Published Date: February 08, 2022
doi: 10.17303/ejmrc.2022.4.101
Citation: Iqra jan (2022) Statins in Chronic Obstructive Pulmonary Disease (COPD): A Feasibility Study to Control Frequent Exacerbations Needing Hospitalization in Kashmiri Population. Eur J Med Res Clin Trials 4: 1-19
Abstract
Introduction: Chronic obstructive pulmonary disease (COPD) is the leading inflammatory obstructive lung diseases responsible for morbidity and mortality around the globe. Current treatment for COPD is for symptomatic relief other than targeted one. Statins have many pleotropic effects like anti-inflammatory and anti-oxidative properties, in addition to decrease cholesterol levels. These features paved the way for their use in various inflammatory diseases including COPD.
Objectives: To study the effect of two different doses of statin therapy on the frequency and severity of exacerbation of COPD and changes in spirometry and lung specific inflammatory biomarkers.
Materials and Methods: 172 COPD out of 200 enrolled patients were selected for the study. Participants were categorized into three groups based on different treatment doses taken and were observed for six months period. Various clinical and laboratory parameters were evaluated pre and post treatment intervention and their correlation was done with the help of different statistical tools.
Results: Number of patients in group A were 54 (31%), 49(28.5%) in group B and 69(40%) in group C. Hospitalization because of exacerbation was required by 37 out of 172 patients, with the maximum incidence seen in group C (n=19;51.4%). Comparison of overall pre and post intervention CAT score and Levels of IL-6 post intervention across the three groups A, B and C, and mean BODE score and IL-8 levels between two treatment groups, A, C and B, C were statistically significant (p < 0.05).
Conclusion: Statins may be regarded as an innovative and much required additional treatment scheme in COPD patients particularly in Kashmir region where climatic as well as socio-economic features augment to the patient load.
Keywords: COPD; Statins; Exacerbation; Hospitalization; Inflammation
Introduction
Chronic obstructive pulmonary disease (COPD) is a type of major respiratory illness that can be prevented and treated with proper medical care. In COPD, there is an extensive evidence of clinical guidelines that let medical practitioners accumulate information and apply best knowledge to their medical practice [1]. Future developments and advancements in this field at molecular level and improvement of new drug therapies will definitely lead to superior therapeutic involvements. [2]
The characteristics of COPD are poor reversibility of airflow which results from chronic inflammation caused due to tobacco smoking [2]. It usually deteriorates as time passes, with classical symptoms of breathlessness, cough and production of sputum [3]. It happens as a consequence of the collective effects of smoking and genetic predisposition. Smoking alone contributes for ~85% of COPD cases, as it proceeds with abundant inflammation all over the respiratory tract and the pathological alterations representative of COPD establish in the pulmonary vasculature, peripheral small airways, proximal large airways [4]. Furthermore, cigarette smoke inhalation results in enormous exogenous oxidant burden on the lung from Reactive Oxygen Species (ROS), which disables several anti-protein mediators mostly α1- antitrypsin causing acquired α1- antitrypsin deficiency [5,6]. Tobacco smoking is the utmost cause of COPD with several other elements like air pollution and genetic susceptibility having a role to play [7]. Fumes from inside homes being substantial source in various countries [6].
Predominance of COPD worldwide ranges from 4-6% (8). Overall Indian prevalence is up to 4.1% with 5% among males and 3.2% among females [9]. Kashmir reported increased incidence of COPD about 7.5% in smokers and 10.5% in people residing in less ventilated homes [10]. Less ventilation of cooking fires, often driven by biomass fuels or coal, leading to indoor air contamination and is utmost causes of COPD among developing countries [11]. An increased prevalence of Chronic Bronchitis (12%) was observed in Gujjar families of the rural area of Kashmir valley [12].
Several studies show a consistent dependency between severity of COPD and primarily C- reactive protein (CRP), biomarkers of systemic inflammation [13,14]. This link is supposed to show an inverse relationship between forced expiratory volume in first second (FEV1) and these biomarkers [15-17]. As per the GOLD Guidelines, COPD diagnosis can be established by a fixed spirometric ratio of post bronchodilator FEV1 and FVC below 0.7 [18].
All the present therapies are hired from asthma and adjusted for COPD, although the fundamental inflammatory pattern in asthma is dissimilar [19]. Currently for treating COPD short and long acting β- agonists are used for relaxing smooth muscle and dilate airways. The response for bronchodilator to this treatment is noticeably less in COPD because of emphysema and small airway fibrosis secondary to matrix remodeling [20]. Thus the treatment of COPD is mainly used for symptomatic relief and improvement in tolerating exercises. Now the understanding regarding COPD has progressed, not only affecting the lungs but being a complex, heterogeneous and generalized disease among aging individuals [21]. Thus COPD cannot be described as a disease limited to lungs, as it has extensive influence on overall health status and FEV1 is not only a lung function factor for ranking COPD severity but also an indicator of earlier death from any disease [22].
Of late statins have arisen as a promising disease revising mediators in COPD [23]. Apart from properties of decreasing cholesterol levels like restoring of vascular functions, antioxidant, anti-inflammatory and anti thrombogenic actions, they possess other pleiotropic effects also [24,22]. The logic for their use in COPD somewhat arises from the fact that COPD pathogenesis arises from inflammation [25] and insistent systemic inflammation is present even in patients with stable COPD without any history of current smoking [26]. The anti-inflammatory effects of statins describe their role in reduction of mortality and morbidity in coronary artery diseases because of their cholesterol lowering effects (which is pleiotropy) [27].
Even though randomized trials are yet to be reported, there is information from several studies that statins might lessen mortality and morbidity in COPD patients. Additional possible paybacks contain a reduced drop in FEV1 and reduced threat of lung cancer [28]. Maximum of the existing data is based on observational studies and there is necessity for ingenious Randomized Controlled Trials, to assess the influence of statins on consequences in COPD population.
Material and Method
Study site
This study was approved by the Institutional Ethics Committee (IEC) of SKIMS Srinagar. This study was piloted in the Departments of Clinical Pharmacology, General Medicine and Immunology and Molecular Medicine SKIMS Srinagar, Kashmir. Patients diagnosed with respiratory diseases visiting our tertiary care hospital were selected for the study cohort after taking a proper informed consent.
Sample size determination
To detect the effect of clinical and laboratory outcome measures of different doses of statin, sample size of 200 subjects were calculated for this research, which was based on the estimated 9% incidence of COPD in Kashmir with anticipated confidence level of 0.05 and margin of error 3%.
Laboratory analysis
Quantitative levels of interleukin-6 (IL-6), interleukin-8 (IL-8) and C Reactive Protein (hsCRP) were measured from serum by ELISA. The biomarkers were measured before and then six months after intervention..
Inclusion and Exclusion criteria
Inclusion criteria
a. Patients clinically diagnosed with COPD as per GOLD criteria
b. Patients who had atleast one or more episodes of acute exacerbations needing emergency hospital visits.
c. Patients using supplementary oxygen and corticosteroids for respiratory problems.
Exclusion criteria
a. Population who had not any history of COPD as per GOLD criteria.
Randomisation
Participants in the study were assigned into comparison groups (A, B, C) on the basis of chance (random) process characterized by unpredictability. For this study based on three intervention groups (A, B, and C), six blocks were created as ABC, ACB, BAC, BCA, CAB, and CBA. The block Randomisation was done on the basis of Standard Randomisation Block method.
Intervention
Apart from conventional treatment of COPD, the patients were classified as group A (taking 40mg Atorvastatin), group B (taking 10mg of Atorvastatin) and group C (controls). A single daily oral dose at bed time to be taken by patients was advised for a period of six months. After six months patients were called for observing consequences (clinical and laboratory outcomes) as well as any Adverse Drug Reactions (ADRs). Any ADRs detected were subjected to casuality assessment and categorization according to WHO Scale before reporting to ADR Monitoring Center (AMC); Department of Clinical Pharmacology SKIMS. The criteria for selecting Statin doses was based on American college of cardiology (ACC) and American Heart Association (AHA) classifications of moderate and high intensity drugs.
Allocation concealment
For each participant assignments was placed in sequentially numbered, sealed opaque envelopes containing tablets (Atorvastatin 10 mg or 40 mg or placebo identical in appearance) to be taken orally daily one envelope for four weeks and proper reporting was done with randomized trial.
Blinding
Blinding was strictly adhered to investigators and participants both were kept blind to any assignment. Interventionist was not involved in conduct of RCT at any stage except for unmasking concealment to interpret results after completion of the RCT.
Compliance Monitoring
For compliance monitoring, patients were frequently but un-announcingly called to attend the study site along with their remaining assignments. Interviews regarding drug intake were held in detail. At the same time remaining tablets of their assigned treatment were counted. In order to remove the adverse influences of 24 hour frequency and cost on the patient’s compliance to treatment regimen, once daily drug dose (least frequency) provided free of cost, further helped in improving the compliance
Outcome assessment:
Patients were followed and assessed after six months of continued intervention therapy for primary and secondary outcome trials measured by BODE INDEX variables and COPD Assessment Test score according to predetermined set of criteria.
BODE INDEX: The BODE index, incorporates body mass index, airflow limitation (forced expiratory volume in one second), dyspnoea and 6-min walk distance, for prediction of mortality in chronic obstructive pulmonary disease (COPD).
Statistical Analytical Methods
Bivariate analysis, Chi square test, Student’s t-test, one way ANOVA, Multivariate analysis, intention to treat analysis (ITTA) strategy and Last Observation Carried Forward (LOCF) method were used at appropriate places. Analysis was done using standard statistical softwares like SPSS and Minitab.
Results
Demographic characteristics of the study cohort
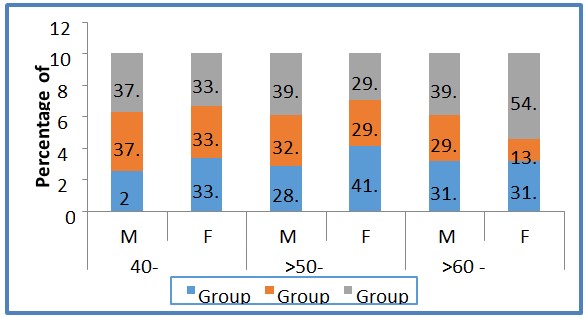
Treatment allocation groups A, B and C were randomized for 172 patients diagnosed with COPD, achieving the GOLD criteria of COPD, with the age group of 40- 70 years, irrespective of gender and smoking status. Comparison of various demographic characteristics are shown in Figure 1.
The rural population comprised of 88 patients (68 male and 22 female), whereas we had 84 patients from urban regions of Kashmir (62 male and 22 females). There was no significant association between the number of patients and their geographical location. Present status of smoke exposure or dependence discloses that out of 172 patients, 50 were smokers, 112 were ex-smokers and 10 were non-smokers. All the 112 ex-smoker patients were exposed to hookah smoke, 30 ex-smokers had an exposure to hookah as well as cigarette smoke, however 15 had exposure to hookah, smoke and biomass fuel and 3 ex-smokers had exposure to hookah, cigarette, biomass fuel and occupational smoke. For acute exacerbation events throughout the study period, the number of patients who required hospitalization were 37 out of 172, with the maximum incidence seen in group C (n=19;51.4%), followed by group B (n=13;35.1%). Group A had least frequency (n=5;13.5%), keeping in consideration that group A took highest dose of statins (40mg) compared to group B, thus clearly demonstrating (Table 2).
Discussion
Kashmir has extended winter time with down pouring of snow thus intensifying the threat of COPD [14]. This study investigates the role of statins in COPD patients which is carried out for the first time in Kashmiri population.
The eligibility for inclusion criteria was fulfilled by 172 out of 200 patients comprising of 130 and 42 males and females respectively, which were arranged into three blind treatment allocation groups A, B and C. Majority of males in this study may be explained for more smoking habits among them. India recorded 11.76:1 male to female ratio of smoking [29]. Several studies have recognized male gender and later ages as elements responsible for COPD (9, 30). This affiliation has been endorsed to the higher predominance of smoking among males and collective outcomes of smoking and other exposures with increasing age [2, 31, 32]. Majority of patients were in the age group of 60 – 70 years for all the three treatment groups (n=108,) which is in acquaintance with other studies [11,33]. COPD is more prevalent among people with age more than 65yrs affecting 34-200 out of 1000 people [34]. COPD is the prime cause of hospitalization among older population in US [34]. Nearly equivalent predominance of 88 patients (66 male and 22 female) from rural areas and 84 (62 male and 22 female) from urban localities of Kashmir valley recommends the common cause of exposure regardless of variance of regionality within the valley. An incidence of 7.55% in smokers and 10.56% in people living in poorly ventilated houses was reported by a study conducted in urban areas of Kashmir [10]. Thus puts forth that tobacco smoking being the imperative risk factor for COPD in Kashmir. In this study we had 29.1% smokers, 65.1% ex-smokers and 5.8% non-smokers.
In this study age at the onset of disease for 113 patients was between 40 and 59 years and for 59 patients age was 60 years or above. During the course of COPD the most common symptoms were cough, dyspnea, breathlessness and variable number of acute exacerbation usually deteriorating during winters and poorly ventilated and crowded spaces.
During this study period 37 patients needed hospitalization for the acute exacerbation episodes with the incidence of 5 (13.5%), 13 (35.1%) and 19 (51.4%) patients from groups A, B and C respectively (Table 1). These findings suggest that statins may avert or at least lessen the incidence of acute episodes of COPD needing hospital admissions.
On comparison of CAT score before and after intervention of statins for 6 months we observed a statistically significant improvement in group A which received maximum dose of statins. Also Post Hoc analysis revealed a highly statistical significance between the group taking maximum dose of statins (group A) and the group taking routine medications for COPD (group C) (p<0.05) (Table 2).
For all the three treatment group of patients A, B and C we observed comparable Pre intervention FEV1 score and post intervention FEV1 score showed a remarkable change although not significant, thus pointing towards higher dosage and prolonged use of statin therapy for overall beneficial effects in patients (Table 3). However FEV1 when taken along with additional factors for disease diagnosis in the BODE Score illustrates statistically significant change (Table 4). Changes observed in the BODE score across the three groups after the subsequent intervention for six months were statistically significant (p<0.05). A statistically significant change was observed in the post intervention mean BODE score between group A and group C and group B and group C (p<0.05). There is a strong correlation between mortality and even cardiac death in COPD patients and rate of decline of FEV1 [35]. In this study lesser rate of decline for six months period was observed which was statistically insignificant (p>0.05), which points towards higher dosage and prolonged use of statin therapy for overall beneficial effects in patients.
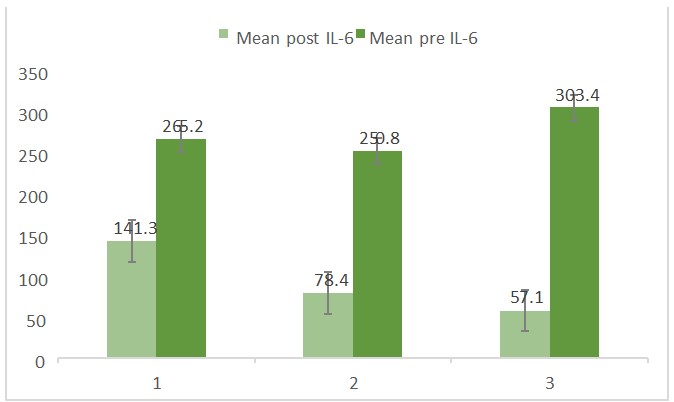
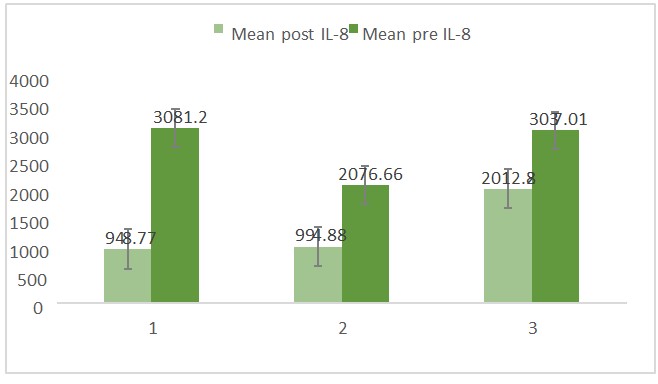
Currently inflammation is regarded as main stimulus (36) for COPD and statins have an array of pleotropic effects like anti-inflammation and latest evidence puts forth that statins lessen inflammatory effects [37,38]. In this study, patients reveal significant rise of inflammatory markers like IL-6, hsCRP and IL8 linked with the inception of this malady, and subsequently six months after intervention with statins a noticeable decrease was observed in the hsCRP concentration of the test groups as compared to controls after receiving 40 mg of statins than 10mg of statins daily for six months (p>0.05). From these findings one can infer that the advantageous outcomes of statins on hsCRP concentration is more seen at consistent advanced doses than at lesser doses.
Higher levels of pro inflammatory cytokines like IL-6 and CRP was observed to be linked with lower FEV1 (39, 40). Several studies have shown that COPD patients have raised concentration of serum CRP than healthy controls which can display the disease severity [41,42].
Levels of inflammatory cytokines (IL-6, IL-8) were significantly lowered after the use of statin therapy for six months period (A vs B p>0.05) when matched with controls or group C (A vs C p<0.05), (B vs C p< 0.05, table 5, 6). The different dosages of drug within the two test groups A and B (40 mg and 10 mg) did not change much the effect between these two groups. By intervention of the statins, progress in the levels of the inflammatory cytokines responsible for COPD has been witnessed.
Data generated from this study may form basis for making statins as a mandatory component in the treatment protocol of the diseases and an initiative to make it available in hospital formularies for this indication besides its other pharmacological indications. Drug safety with compliant low single daily dose and efficacy makes it appropriate and optimum treatment option for the Disease.
In view of above findings we can interpret that Statin therapy for a sustained periods appears to provide general advantage in improving the laboratory as well as clinical parameters in COPD patients
Conclusion
The purpose of this study was to investigate the consequence of supplementary treatment on the clinical severity of COPD patients from Kashmir. This study is aimed to positively contribute and validate significance and underlying principle of adding statins to the current treatment choices for COPD.
This study confers that statins have noteworthy supplementary paybacks in COPD where raised levels of numerous inflammatory mediators is common and statins are meant to target the pulmonary inflammation. Current study discloses that statins have a substantial advantageous result not only on CRP but also on other essential inflammatory markers. Thus, statins may characterize an innovative and much required additional treatment scheme in COPD patients particularly in Kashmir region where climatic as well as socio-economic features have proven to augment to the quantity of patients and furthermore degrades the situation of those previously suffering from this sickness.
- O’Donnell DE, Aaron S, Bourbeau J (2007) Canadian Thoracic Society recommendations for management of chronic obstructive pulmonary disease – 2007 update. Can Respir J 14: 5-32B.
- Salvi S (2014) Tobacco smoking and environmental risk factors for chronic obstructive pulmonary disease. Clin Chest Med 35: 17-27.
- Vestbo (2013) Jørgen Definition and Overview. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease. Global Initiative for Chronic Obstructive Lung Disease 2013: 1–7.
- Halvorsen B, Otterdal KT, Onstad SA, Ukrust P (2008) Smoking and inflammation: Their synergistic roles in chronic disease. Curr. Cardiovasc. Risk Rep 2: 446-51.
- Roth M (2008) Pathogenesis of COPD. Part III. Inflammation in COPD. Int. J. Tuberc. Lung. Dis 12: 375-80.
- Langen RCJ, Korn SH, Wouters EFM (2003) ROS in the local and systemic pathogenesis of COPD. Free Radic Biol Med 35: 226–35.
- Decramer M, Janssens W, Miravitlles M (2012) Chronic obstructive pulmonary disease. Lancet 379: 1341–51.
- Nazir SA, Erbland ML (2009) Chronic obstructive pulmonary disease: an update on diagnosis and management issues in older adults. Drugs Aging 26: 813-31.
- Jindal SK, Aggarwal AN, Chaudhry K (2006) Asthma epidemiology study group. A multicentric study on epidemiology of COPD and its relationship with tobacco smoking and environmental tobacco smoke exposure. Indian J Chest Dis Allied Sci 48: 23-7.
- Akhtar MA, Latif PA (1999) Prevalence of chronic bronchitis in urban population of Kashmir. J Indian Med Assoc 97: 365-6.
- Kennedy SM, Chambers R, Du W, Dimich-Ward H (2007) Environmental and occupational exposures: do they affect chronic obstructive pulmonary disease differently in women and men? Proceedings of the American Thoracic Society 4: 692–4.
- Qureshi KA (1994) Domestic smoke pollution and prevalence of chronic bronchitis/ asthma in a rural area of Kashmir. Indian J Chest Diseases & allied sciences 6: 61-70.
- Sin DD, Man PSF (2003) Why are patients with chronic obstructive pulmonary disease at increased risk of cardiovascular disease? The potential role of systemic inflammation in chronic obstructive pulmonary disease. Circulation 107: 1514-9.
- Shaaban R, Kony S, Driss F (2006) Change in C-reactive protein levels and FEV1 decline: a longitudinal population-based study. Resp Med 100: 2112–20.
- Yende S, Waterer GW, Tolley EA (2006) Inflammatory markers are associated with ventilatory limitation and muscle dysfunction in obstructive lung disease in well functioning elderly subjects. Thorax 61: 10–6.
- Walker RE, Wilk JB, Larsen MG (2008) Systemic inflammation and COPD: the Framingham Heart Study. Chest 133: 19–25.
- Sin DD, Man SFP (2008) Interluekin 6. Chest 133: 4-6.
- Wouters EF, Reynaert NL, Dentener MA, Vernooy JH (2009) Systemic and local inflammation in asthma and chronic obstructive pulmonary disease: is there a connection? Proc Am Thorac Soc 6: 638–47.
- Spurzem JR, Rennard SI (2005) Pathogenesis of COPD. Semin. Respir. Crit. Care Med 26: 142-53
- Yvonne Nussbaumer-ochsner, Klaus F Rabe, Wouters EF, Reynaert NL, Dentener MA, et al. (2011) Systemic Manifestations of COPD. Chest 139: 165-73.
- Young RP, Hopkins RJ, Eaton TE (2007) Forced expiratory volume in one second: not just a lung function test but a marker of premature death from all causes. Eur Resp J 30: 616–22.
- Barnes PJ, Shapiro SD, Pauwels RA (2003) Chronic obstructive pulmonary disease: molecular and cellular mechanisms. Eur Respir J 22: 672-88.
- Palinski W (2001) New evidence for beneficial effects of statins unrelated to lipid lowering. Arterioscler Thromb Vasc Biol 21: 3-5.
- Bonetti PO, Lerman LO, Napoli C, Lerman A (2003) Statin effects beyond lipid lowering: are they clinically relevant? Eur Heart J 24: 225-48.
- Gan WQ, Man SFP, Senthilselvan A (2004) Association between chronic obstructive pulmonary disease and systemic inflammation: a systematic review and a metaanalysis. Thorax 59:574-80.
- Schonbeck U, Libby P (2004) Inflammation, immunity, and HMG-CoA reductase inhibitors: statins as anti-inflammatory agents? Circulation 109: 1118–26.
- Young RP, Hopkins R, Eaton TE (2009) Potential benefits of statins on morbidity and mortality in chronic obstructive pulmonary disease: a review of the evidence. Postgrad Med J 85: 414-21.
- MR Miller, J Hankinson, V Brusasco, F Burgos, R Casaburi, et al. (2000) ATS/ERS task force: standardisation of lung function testing’’Edited by V. Brusasco, R. Crapo and G. Viegi Number 2 in this Series Standardisation of spirometry.
- International Institute for Population Sciences. India (1999) National Family Health Survey (NFHS-2). Mumbai, India: International Institute for Population Sciences; 20007.
- Jindal Kim DS, Kim YS, Jung KS, Chang JH, Lim CM,Lee JH, et al. (2005) Prevalence of chronic obstructive pulmonarydisease in Korea: a population based spirometry survey.Am J Respir Crit Care Med 172 : 842-7.
- Tan WC (2005) Chronic obstructive pulmonary disease: epidemiology. In: Ip M, Chan Yeung M, Lam WK, Zhong NS, editors. Respiratory medicine - an Asian perspective. Hong Kong: Hong Kong University Press 2005: 61-72.
- Jindal SK, Gupta D, Singh AJ (1994) Indices of morbidity and control of asthma in patients exposed to environmental tobacco smoke. Chest 106: 746-9.
- Vestbo Jørgen (2013) Introduction. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease. Global Initiative for Chronic Obstructive Lung Disease, 2013: 8-15.
- Poole PJ, Chacko E, Wood-Baker RW, Cates CJ (2006) Influenza vaccine for patients with chronic obstructive pulmonary disease". In Poole, Phillippa. Cochrane Database Syst Rev: CD002733.
- Statins and the Lung: Hope or Hype? Indian J Chest Dis Allied Sci 53: 79-80.
- Pauwels RA, Buist AS, Calverley PM, Jenkins CR, Hurd SS (2001) Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) workshop summary. Am J Respir Crit Care Med 163: 1256–76.
- Altose (2003) Aproaches to slowing the progression of COPD. Curr. Opin. Pulm. Med 9: 125-30.
- Feldman C (2009) The role of statins in respiratory diseases. Clin Pulm Med 16: 95100.
- Chang SS, Vaz Fragoso CA, Van Ness PH, Fried LP, Tinetti ME (2011) Association between combined interleukin-6 and C-reactive protein levels and pulmonary function in older women: results from the Women's Health and Aging Studies I and II. J Am Geriatr Soc 59: 113-9.
- Mannino DM, Ford ES, Redd SC (2003) Obstructive and restrictive lung disease and markers of inflammation: data from the Third National Health and Nutrition Examination. Am J Med 114: 758-62.
- Schols AM, Buurman WA, Staal van den Brekel AJ, Dentener MA, Wouters EF (1996) Evidence for a relation between metabolic derangements and increased levels of inflammatory mediators in a subgroup of patients with chronic obstructive pulmonary disease. Thorax 51: 819-24.
- Biljak VR, Pancirov D, Cepelak I (2011) Platelet count, mean platelet volume and smoking status in stable chronic obstructive pulmonary disease. Platelets 22: 466-70.

Tables at a glance
Figures at a glance