Postoperative Delirium in Elective Cardiac Surgery is not Associated with Changes in Peripheral Cholinesterases
Received Date: December 27, 2024 Accepted Date: January 27, 2025 Published Date: January 30, 2025
doi: 10.17303/ejmrc.2025.7.101
Citation: Zangl Q, Zinn N, Bergmann A, Hulde N, Hagl C, et al. (2025) Postoperative Delirium in Elective Cardiac Surgery is not Associated with Changes in Peripheral Cholinesterases. Eur J Med Res Clin Trials 6: 1-14
Abstract
Background: Postoperative delirium (POD) is a common complication following elective cardiac surgery, with significant implications for patient outcomes and healthcare costs. The pathophysiology of POD is multifactorial, involving neuroinflammation and imbalances in the central cholinergic system.
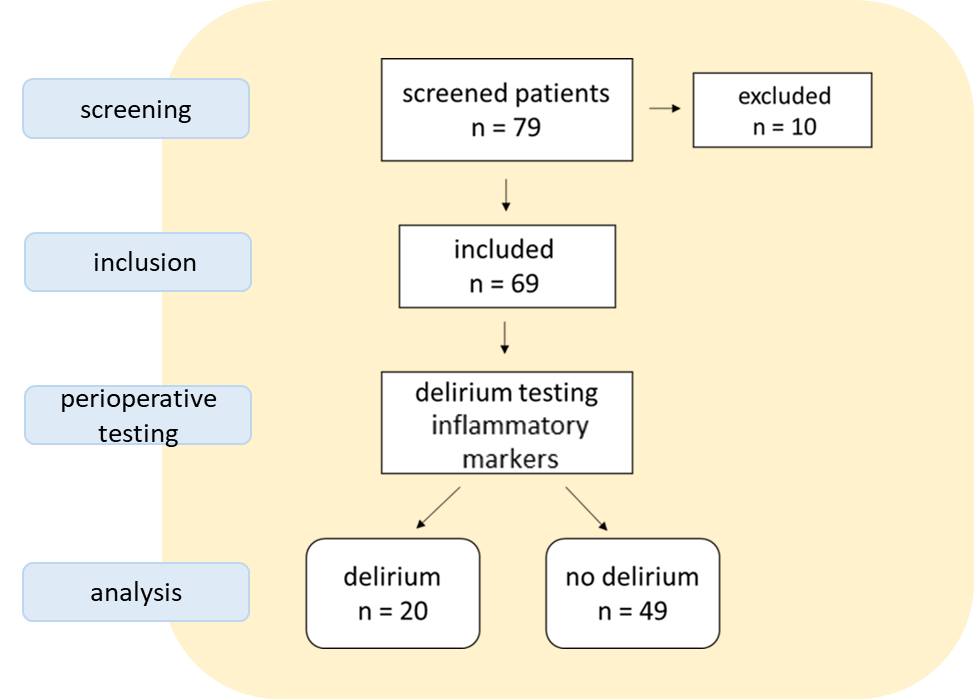
Methods: This study evaluated the relationship between peripheral cholinesterase (AChE and BChE) activities and POD occurrence in 69 cardiac surgery patients (n=20 with delirium/ n=49 without). Cholinesterase levels were measured at six perioperative time points, and their correlations with POD and inflammatory parameters (CRP, IL-6, leukocytes) were assessed.
Results: Neither AChE nor BChE values differed significantly between patients who experienced delirium and those without delirium (all p>0.05) during 6 perioperative time points. The course of AChE values of patients with POD was stable (n=20; p=0.266), whereas the course of perioperative AChE differed significantly in non-delirant patients (n=49; p=0.005). BChE values dropped significantly in both groups: both in the group of patients with POD (n=20; p<0.001) and in the group without POD (n=49; p<0.001) the BChE values fell significantly in the postoperative course. Correlations between AChE and inflammation parameters (leukocytes, CRP and Il-6) were not significant, independent of the occurrence of delirium (all p >0.05). The values of BChE in correlation to inflammatory parameter was non-significant in delirious patients, whereas postoperative leukocyte values correlated significantly with the absence of delirium (day1 p<0.001 [n=48]; day2: p=0.024[n=48]; day3: p=0.005[n=47]).
Results: No significant differences in cholinesterase levels were found between delirious and non-delirious patients, nor were there significant correlations with inflammatory markers. While BChE levels showed perioperative decreases, these changes were not specific to POD.
Conclusion: As a clinical implication, it must be concluded that the measurements of cholinesterases have limited utility in predicting POD. Furthermore, cholinesterases seem to have limited value for the management of the course of POD and possible associations with inflammation as standalone biomarkers. However, larger studies are necessary to explore their potential role in indicating inflammatory states.
Keywords: Postoperative Delirium; POD; Cardiac Surgery; Cholinesterase; Ache; Bche; Inflammatory Parameters; CNS
Introduction
The negative consequences of postoperative delirium (POD) got increasing attention during the last 2 decades. As is well known, cardiac surgical patients are at the highest risk of developing POD [1]. It is well established that patients who suffer from POD are exposed to higher morbidity and mortality risks, require significantly more medical care and consequently require far above-average financial outlay. These issues apply both inside and outside of hospitals [2]. Factors that seem to influence POD development are the invasiveness of the surgical procedure (especially with the heart-lung machine), anesthesia, number of preexisting diseases with their associated medications (especially with anticholinergic effects) and of course, the foreign environment, in which associated, individual stress reactions take place [3,4].
Increasing evidence points to disturbances in the delicate transmitter balance in the central nervous system (CNS) as the common final stretch during POD development. In particular, the changes during POD seem to be a consequence of inflammatory reactions and their effects on the transmitter balance in CNS [3,5]. The cholinergic system with the neurotransmitter acetylcholine (ACh) seems to play a pivotal role here. A particular challenge is that indicators of changed neuronal activity in the body’s periphery (“biomarkers”) are very difficult to find and to measure, especially the very unstable ACh. Therefore, as a reference for ACh effects, its degrading enzymes acetylcholinesterase (AChE) and butyrylcholinesterase (BChE) from the blood are analyzed here [5,6,7].
The underlying pathophysiological concept assumes that the central cholinergic system plays a pivotal role in regulating inflammatory responses in the brain (“cholinergic deficiency hypothesis”). A peripheral stimulus (surgery) induces an inflammatory reaction with consecutive release of inflammatory mediators into the blood, which cross the blood brain barrier and activate microglia there. A complementary hypothesis states the microglial “sensing” of inflammation takes place via the vagus nerve. The centrally activated inflammation can then lead to mentioned transmitter imbalances and thus promote the phenotypic phenomena, like POD. The hypothesis further assumes that lack of inhibition via the central cholinergic pathways can aggravate the inflammatory response in the brain (through missing microglial inhibition). Obviously, central cholinergic inhibition should only work to a very limited extent if the cholinergic system has already been “shut down” pharmacologically afore. Evidence points to altered changes of AChE and BChE in serum as possible and promising biomarkers, reflecting central cholinergic activity as a POD “biomarker” [6,7].
The aim of this study was to evaluate effects of elective cardiac surgery on peripheral concentrations of cholinesterases as indicators of centrally acting acetylcholine depending on POD and associated postoperative inflammation. Furthermore, POD-associated risk factors, like age, anticholinergic drug load, comorbidity, preexisting central nervous diseases were explored and their association with POD after cardiac surgery analyzed.
Materials and Methods
This investigation is a sub study of the CESARO project, published in 20197. Here, we analyze only the cardiac surgical patient population, which was operated in Munich (LM-university, Munich, Germany). The ethical commission signed the investigation afore (LM-university Munich ethical board ref.: 558-13). A total of 79 patients who underwent elective cardiac surgery using a heart-lung machine were included [7].
The Inclusion Criteria were
The Exclusion Criteria were
- Patients undergoing elective cardiac surgery using a heart-lung machine
- Age ≥ 18 years
- Written declaration of consent
- Patients with known pseudocholinesterase (BChE) deficiency
- Employment at the respective study centers
- Lack of consent to store and pass on pseudonymized data
- Placement in an institution following a court or official order
- The presence of illiteracy
- Insufficient English or German language skills
- Presence of severe hearing or visual impairment
- Participation in another prospective clinical intervention study
- Age < 18 years
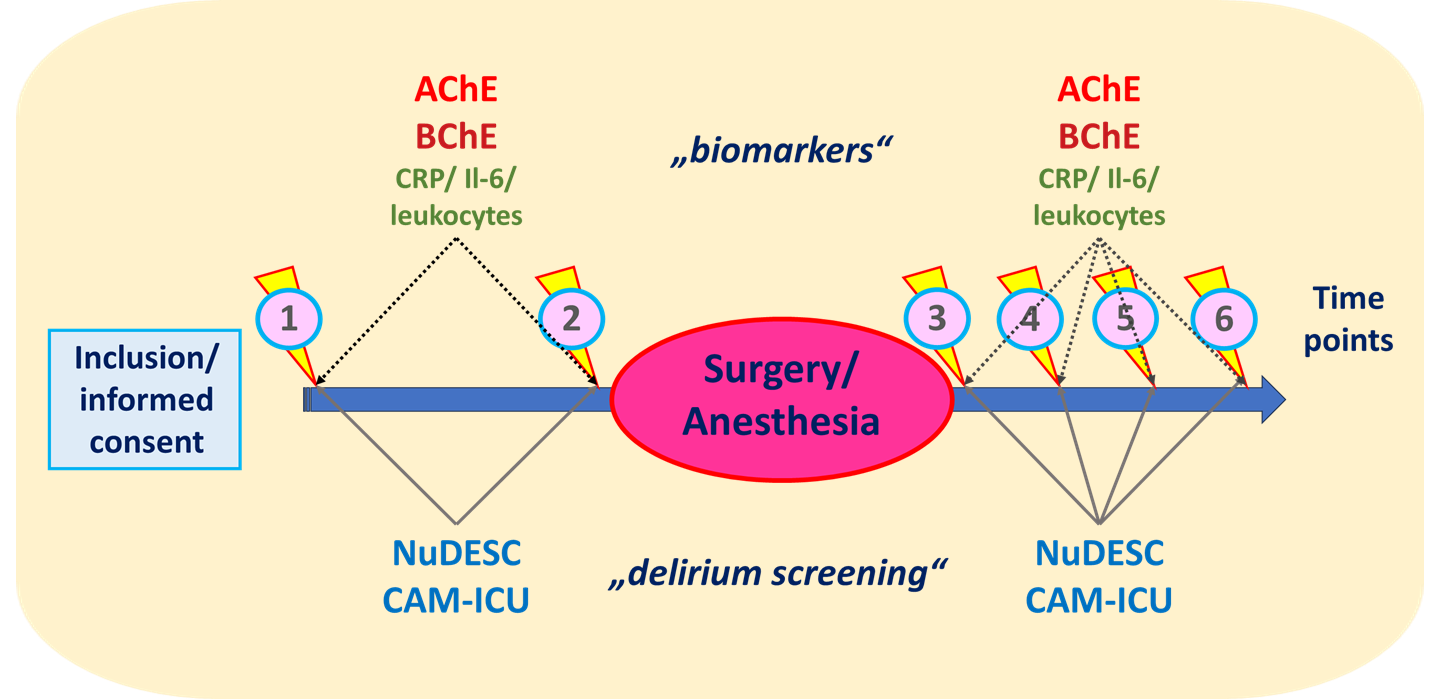
After preoperative screening for eligibility, an explanation of the timing, content and purpose of the study was provided at least 24 hours before the start of the operation and confirmed by a written informed consent form. After inclusion in the study, the basic characteristics, delirium screening (Nu-DESC and CAM-ICU) [8] and the measurement of AChE and BChE activity in whole blood (“baseline”) were carried out preoperatively [9-11].
After the operation, five additional measurement points were defined for AChE, BChE, CAM-ICU and Nu-DESC: after induction of anesthesia, after admission to the intensive care unit and on the first, second and third postoperative day. In addition to that, serum inflammatory parameters, as C-reactive protein (CRP), interleukine-6 (Il-6) and leukocyte concentrations were documented at each measurement point [12]. This resulted in a total of six measurement points. All patients had the opportunity to discontinue the study at any time.
Measurement of peripheral cholinesterase activity was performed as point-of-care testing, using 10 μl of capillary blood and a validated photometric test (ChE Check Mobile; Securetec Detektions-Systeme AG, Neubiberg, Germany) [10,11]. According to the instructions from the manufacturer, measurements were performed at six time points for each patient: at least 1 day prior to operation, shortly before anesthesia induction, on admission to recovery room or PACU, on discharge from recovery room or PACU, 1 day after surgery, and 3 days after surgery.
According to the manufacturer's specifications, the reference range for AChE was 26.7- 50,9 U/g Hb and for BChE: 2300 - 7000 U/l. To deal with missing values, we included three defined measurements (time points) into the analysis. An overview of the included measurements is listed below (figure 2). Both AChE and BuChE activities were quantified at each time point [10,11].
For detection of POD, Nursing Delir Score (Nu-DESC) and CAM-ICU, as a highly validated diagnostic tool, were done one day before the operation (baseline measurement), on the operation day before the induction of anesthesia, in the recovery unit before discharge, on the first and third postoperative day. Nu-DESC assesses five dimensions: orientation, behavior, communication, illusion/hallucination, and psychomotor retardation [8]. The symptoms are rated on a three-point scale. A score of two or more cumulative points indicates delirium. The Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) is an additional tool for assessing delirium in patients in the intensive care unit [8].
Additional recorded parameters were: age, height, weight, body mass index, gender, medical history (preoperative diagnoses, accompanying diagnoses, smoking and alcohol history, ASA status and allergies) and drug therapy (long-term medication and premedication). The anticholinergic potential of the long-term medication was determined using the Anticholinergic Drug Scale (ADS) [9,12].
Further parameters were: duration of the operation and anesthesia, intraoperative medication, anesthesia procedures, post-ventilation time, amount of blood loss (and amount and type of blood products), duration of extracorporeal circulation (heart-lung machine), aortic clamping time, duration of hypothermic cardiac arrest, amount and type of cardioplegia solution administered.
Statistical Analysis
The statistical analysis was carried out using the software “R”, version 4.4.1.
All data were first examined for normal distribution. For this purpose, the Kolmogorov Smirnov test and graphic representations (QQ plots and histograms) were used. According to the presence of normal distribution, the data were then examined for significant differences (with a set level of p<0.05).
First, baseline values and association with POD were examined. The independent variable age using a t-test (binary values, normally distributed), other, categorial baseline characteristics (ASA-score, gender, ADS-score, smoking and alcohol-intake - all normally distributed) using a Fisher´s exact test. Finally, the association between the euroscore and POD was carried out using the Mann-Whitney-U test (due to non-normal distribution).
Differences in AChE/BChE concentrations between patients with POD and without were then examined with the independent sample t-test (with normal distribution) or the Mann Whitney U test (without normal distribution) was used.
Then, using analysis of variances (“anova”; dependent samples with repeated measurements) and subsequent Bonferroni analysis (for α correction), the course of the enzymes AChE/BChE was carried out in patients with and without POD.
Finally, the metrically scaled inflammation parameters (leukocytes, CRP and IL-6) were analyzed using Pearson correlation analysis with AChE and BChE for normally distributed values (and Spearman correlation without normal distribution) [13].
Results
Baseline Characteristics
Mean age of the patients was 65.65 (±10.46) years. Patients with delirium were 65.6 (± 8.5) years, those without POD 65.6 (±11.2) years (without significant difference: p=0.979). Gender distribution showed 50 (72.5%) male and 19 (27.5%) female patients. Of them 17 male (34%) and 3 female patients (15.8%) developed POD, without significant difference (p=0.234).
Neither ASA classification (p=0.664), nor ADS scale (p>0.05), nor euroscore (p=0.123) nor regular smoking (p=0.301) showed significant differences. Only regularly increased alcohol consumption (more than 12g/d for women or 24g/d for men) showed significantly higher incidences of delirium (p=0.032).
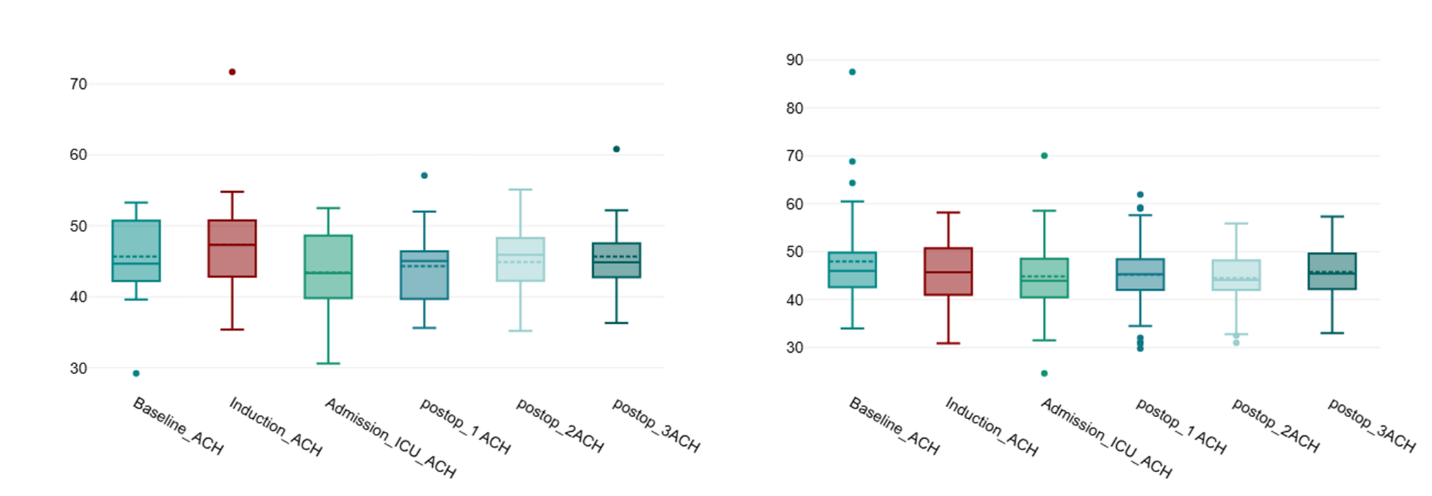
Ache Values Between Delirious and Non-Delirious Patients
From the data it can be concluded that the AChE values of delirious patients did not differ significantly from non-delirious patients (all p-values >0.05).
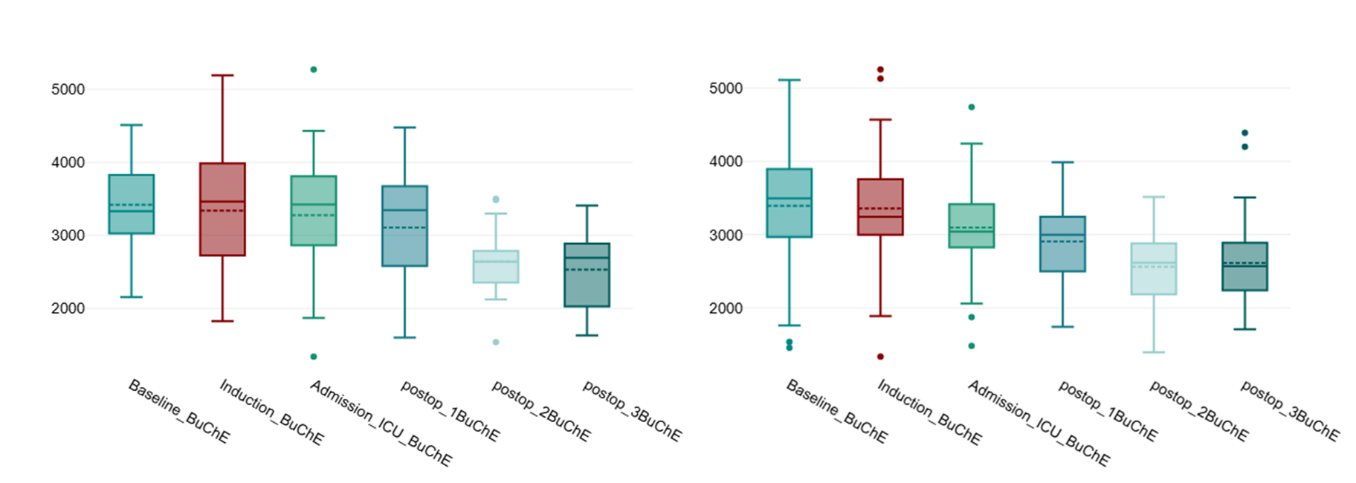
Bche Values Between Delirious and Non-Delirious Patients
From the data it can be concluded that the BChE values of delirious patients did not differ significantly from non-delirious patients (all p-values >0.05).
Course of AChE Values
Ache Values of Patients with Delirium
In patients suffering from delirium, there was no significant change of AChE values in all six perioperative measurements (n=20; p=0.266; effect size η2p = 0.06); reflecting a stable course of AChE values. Consequently, post-hoc (Bonferroni) analysis did not reveal any significant changes between each combination of measurement points (not shown).
Ache Values in Patients without Delirium
In patients without delirium, there was a significant change of AChE values during perioperative measurements (n=49; p=0.005; effect size η2p = 0.07). Further analysis demonstrated significantly lower AChE values after ICU admission in relation to baseline values (p=0.003), however, the other 4 measurements (anesthesia induction and postoperative days 1-3) did not show significant differences (not shown).
Course of BChE Value
BChE Values of Patients with Delirium
In patients with delirium, there was a significant change of BChE values in perioperative measurements (n=20; p<0.001; effect size η2p = 0.33). In relation to baseline values, on the second (p=0.001) and third (p<0.001) postoperative day, BChE decreased significantly. Measurements from anesthesia induction until the first postoperative day did not show any significant differences (not shown).
BChE Values of Patients without Delirium
In patients without delirium, there was a significant change of BChE values in perioperative measurements (n=49; p<0.001; effect size η2p = 0.34), in relation to baseline values, on the first (p=0.005), second (p<0.001) and third (p<0.001) postoperative day, BChE values decreased significantly. The values after anesthesia induction and icu admission did not differ significantly (not shown).
Cholinesterases and Inflammatory Parameters
AChE Correlated with Leukocytes, CRP and Il-6
No significant correlations between AChE, delirium and inflammation parameters (leukocytes, CRP and Il-6) could be found (all p>0.05)
BChE Correlated with Leukocytes, CRP and Il-6
Significant correlations between BChE, delirium and inflammation parameters (leukocytes, CRP and Il-6) could only be found in non-delirious patients: on the first (n=48; p<0.001), second (n=48; p=0.024) and third postoperative day (n=47; p=0.005). Additionally, CRP was significant lower during anesthesia induction in non-delirious patients (n=11; p=0.01). All other correlations did not show significant values (all p>0.05).
Discussion
Cholinesterases (AChE/BChE) play a crucial role in fine adjustment of excitatory neurotransmitter acetylcholine, which is necessary for higher central nervous functions, such as attention, awareness, orientation and goal-oriented thinking [5-7]. Disturbances of this fine balance may occur during operations due to different factors, like anesthetic medications, (i.e. benzodiazepines), direct anticholinergic drugs (i.e. atropine) and the surgical stress response (which is centrally regulated in hypothalamus). The cholinesterase, as a regulator of acetylcholine concentrations, may therefore play a crucial role in the development of postoperative cognitive peculiarities, like POD and POCD. In this study, we investigated serum cholinesterase concentrations (AChE/ BChE) for the correlation with either POD or POCD as bedside measurement in a urological collective for the first time.
This investigation included 69 patients undergoing elective cardiac surgery with the help of the heart-lung machine (non-pulsatile procedure). Overall, it must be stated that in this study no excessive connections could be demonstrated between the occurrence of POD and neither the absolute values of the cholinesterases, nor their courses nor their correlation with the inflammatory parameters, together with POD (which was the basic hypothesis).
Comparable to other working groups 20 patients (29%) suffered from POD [14,15].
There were no significant differences between delirious and non-delirious patients in the basic characteristics. Other studies determined ASA state as an established risk factor for the development of POD [16-18], what we could not confirm. Amazingly, we found no significant correlation between the well-established risk factor age and POD [19], which may be attributed to the relatively low average age of the patients (66 years). The suspected low cholinergic activity in central nervous system due to its drug-induced reduction (“anticholinergic load”) [21] was also not significantly associated with the likelihood of POD. Same was true for Euroscore and POD (risk of heart surgery in adults) [22]. Regular smoking is no established risk factor for the development of POD and we can confirm this with our findings [22]. Although the study situation is still not clear, it is obvious that regular alcohol consumption and its interruption perioperatively may contribute to POD, which we also clearly confirm [23,24].
In this study, no significant changes in the cholinesterases measured peripherally in the blood (AChE and BChE perioperatively at six measurement points) and the probability of POD occurrence could be measured. This study analyzed the cardiac surgery subgroup from the "Cesaro" [25] study. Here too, after adjusting for covariates, no significant association was found between peripheral cholinesterases and the postoperative probability of POD occurrence in a larger, mixed surgical group. We were unable to confirm the tendencies of lower BChE values initially and on the first two postoperative days as well as increased AChE values initially and on both first postoperative days in our cardiac surgical population.
In this study, the course of AChE and BChE was analyzed pre- and postoperatively in order to detect possible up- and down-regulations in relation to POD or, conversely, to detect POD-mitigating properties. According to common hypothesis [26,27], central acetylcholine deficiency seems to correlate with increased peripheral esterase activity.
However, drug inhibition of cholinesterases was not effective in reducing POD in recent trials [26,27]. In line with these findings, the courses of the peripheral cholinesterases only showed significant changes in BChE in delirious patients on the first two postoperative days, but also in non-delirious patients on the 3 postoperative measurements. This could be due to the body's own down-regulation mechanisms in the postoperative setting per se, which appear to be independent of the occurrence of delirium. This is in accordance with recent findings [28].
Finally, we checked the correlation between common inflammatory parameters (leukocytes, CRP and IL-6 in the serum) and their course in the context of peripheral cholinesterases and POD. The current hypotheses regarding the etiology of POD cite an inflammatory reaction occurring in the central nervous system as a relevant factor in its development [29,30]. although the chosen 3 inflammation parameters appear to be suitable for the contexts examined. Only a few significant connections could be found [31]: the BChE reduced on the three postoperative days correlated significantly with the increased leukocyte values in non-delirant patients. The significant lower CRP values in non-delirious patients during anesthesia induction seems to be random, inflammation usually doesn´t occure preoperatively (except endocarditis i.e.). It must be stated that we were unable to determine a clear connection between the course of the common inflammation parameters and the leakage of pod. However, the question naturally remains as to whether peripheral inflammatory parameters are really sufficient to detect sterile inflammatory processes in the central nervous system and their consequences.
It would be beneficial to identify an inflammatory biomarker for POD. However, plasma cholinesterases are influenced by numerous factors, complicating their discriminative ability. Despite this, the data on butyrylcholinesterases suggest they might provide insights into the inflammatory state. Nevertheless, further research involving a significantly larger patient cohort is required to substantiate these findings and refine their clinical relevance.
Limitations
A limitation of the present work is the fact that a rather small collective of only 69 patients could be examined. It must be noted that the work is a sub-collective of the "CESARO" [25] work and unfortunately could not be achieved with the available means and possibilities.
It should also be noted that the evidence for a clear correlation between serum and cerebrospinal fluid cholinesterase is rather low, but was the best possible method for this purpose [15]. Furthermore, it must be mentioned that the clinical analysis of peripheral cholinesterases is the subject of current discussions and is by no means (yet) considered established, but is only being explored for this purpose. The "cholinergic anti-inflammatory pathway" posits that central acetylcholine modulates systemic inflammation via the vagus nerve, indirectly implicating peripheral cholinesterase as a surrogate marker. Data used to underline common hypothesis of neuroinflammation during the pathogenesis of POD largely rely on animal models, in which glial reactions due to common inductors of systemic inflammation (administration of lipopolysaccharide [LPS]) were analysed.
Conclusion
This work is a first attempt to find relationships between cholinesterase concentrations, POD in a cardiac surgical patient population. Further work will be needed in the future to show whether cholinesterase is suitable as a risk marker and therapy companion for patients with POD.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding
This paper was not funded.
Data Sharing
Data available on request.
Author Contributions
VvD conceptualized the study. QZ wrote the manuscript and analyzed the data. VvD and CH also designed the study and supervised the data collection (done by NZ and ES). NZ and ES did the laboratory analysis and field work. NH and AB critically reviewed the manuscript and developed the final version. VvD and CH involved in the development of study protocol. All authors commented on manuscript and approved the final version.
Data availability Statement
The data set that was created during the study is publicly available on request.
- Chen H, Mo L, Hu H, Ou Y, Luo J (2021) Risk factors of postoperative delirium after cardiac surgery: a meta-analysis. J Cardiothorac Surg. 16: 113.
- Gleason LJ, Schmitt EM, Kosar CM, Tabloski P, Saczynski JS, et al. (2015) Effect of Delirium and Other Major Complications on Outcomes After Elective Surgery in Older Adults. JAMA Surg. 150: 1134-40.
- Duning T, Ilting-Reuke K, Beckhuis M, Oswald D (2021) Postoperative delirium - treatment and prevention. Curr Opin Anaesthesiol. 34: 27-32.
- Bramley P, McArthur K, Blayney A, McCullagh I (2021) Risk factors for postoperative delirium: An umbrella review of systematic reviews. Int J Surg. 93: 106063.
- Paunikar S, Chakole V (2024) Postoperative Delirium and Neurocognitive Disorders: A Comprehensive Review of Pathophysiology, Risk Factors, and Management Strategies. Cureus. 16: e68492.
- Yoon BH, Yoo JI, Youn JC, Ha YC (2017) Cholinergic enhancers for preventing postoperative delirium among elderly patients after hip fracture surgery: A meta-analysis. European Geriatric Medicine; 8: 486-91
- Müller A, Olbert M, Heymann A, Zahn PK, Plaschke K, et al. (2019) Relevance of peripheral cholinesterase activity on postoperative delirium in adult surgical patients (CESARO): A prospective observational cohort study. Eur J Anaesthesiol. 36: 114-22.
- Kim S, Choi E, Jung Y, Jang I (2023) Postoperative delirium screening tools for post-anaesthetic adult patients in non-intensive care units: A systematic review and meta-analysis. J Clin Nurs. 32: 1691-704.
- Plaschke K, Thomas C, Engelhardt R, Teschendorf P, Hestermann U, Weigand MA, (2007) u. a. Significant correlation between plasma and CSF anticholinergic activity in presurgical patients. Neurosci Lett. 417: 16-20
- White S, Calver BL; Newsway V, Wade R, Patel S, Bayer A, O´Mahony MS (2005) Enzymes of drug metabolism during delirium. Age Ageing. 34: 603-8.
- Zangl Q, Sprinz B, von Dossow V (2023) Peripheral cholinesterase activity is not correlated with postoperative delirium in urological surgery. J Perioper Pract. 34: 32-8.
- Simone MJ, Tan ZS (2011) The role of inflammation in the pathogenesis of delirium and dementia in older adults: a review. CNS Neurosci Ther. 17: 506-13.
- Panos GD, Boeckler FM (2023) Statistical Analysis in Clinical and Experimental Medical Research: Simplified Guidance for Authors and Reviewers. Drug Des Devel Ther. 17: 1959-61.
- Rudolph JL, Inouye SK, Jones RN, Yang FM, Fong TG, Levkoff SE, Marcantonio ER (2010) Delirium: an independent predictor of functional decline after cardiac surgery. J Am Geriatr Soc. 58: 643-9.
- Plaschke K, Fichtenkamm P, Schramm C, Hauth S, Martin E, Verch M, Karck M, Kopitz J (2010) Early postoperative delirium after open-heart cardiac surgery is associated with decreased bispectral EEG and increased cortisol and interleukin-6. Intensive Care Med. 36: 2081-9.
- Lee, D.Y., Oh, A.R., Park, J. et al. (2023) Machine learning-based prediction model for postoperative delirium in non-cardiac surgery. BMC Psychiatry, 23: 317.
- Wang Y, Zhao L, Zhang C, An Q, Guo Q, Geng J, Guo Z, Guan Z (2021) Identification of risk factors for postoperative delirium in elderly patients with hip fractures by a risk stratification index model: A retrospective study. Brain Behav. 11: e32420.
- Brouquet A, Cudennec T, Benoist S, Moulias S, Beauchet A, Penna C, Teillet L, Nordlinger B (2010) Impaired mobility, ASA status and administration of tramadol are risk factors for postoperative delirium in patients aged 75 years or more after major abdominal surgery. Ann Surg. 251: 759-65.
- Jin Z, Hu J, Ma D (2020) Postoperative delirium: perioperative assessment, risk reduction, and management. Br J Anaesth. 125: 492-504.
- Herrmann ML, Boden C, Maurer C, Kentischer F, Mennig E, et al. (2022) Anticholinergic Drug Exposure Increases the Risk of Delirium in Older Patients Undergoing Elective Surgery. Front Med (Lausanne). 9: 871229.
- Egberts A, Moreno-Gonzalez R, Alan H, Ziere G, Mattace-Raso FUS (2021) Anticholinergic Drug Burden and Delirium: A Systematic Review. J Am Med Dir Assoc. 22: 65-73.e4.
- Ten Broeke M, Koster S, Konings T, Hensens AG, van der Palen J (2018) Can we predict a delirium after cardiac surgery? A validation study of a delirium risk checklist. Eur J Cardiovasc Nurs. 17: 255-61.
- Shah S, Weed HG, He X, Agrawal A, Ozer E, Schuller DE (2012) Alcohol-Related Predictors of Delirium After Major Head and Neck Cancer Surgery. Arch Otolaryngol Head Neck Surg. 138: 266-71.
- Wu X, Zhang N, Zhou B, Liu S, Wang F, et al. (2023) Alcohol consumption may be associated with postoperative delirium in the elderly: the PNDABLE study. BMC Anesthesiol. 23: 222.
- Müller A, Olbert M, Heymann A, Zahn PK, Plaschke K, et al. (2019) Relevance of peripheral cholinesterase activity on postoperative delirium in adult surgical patients (CESARO): A prospective observational cohort study. Eur J Anaesthesiol. 36: 114-22.
- Overshott R, Karim S, Burns A (2008) Cholinesterase inhibitors for delirium. Cochrane Database Syst Rev. 2008: CD005317.
- Lieberman OJ, Douglas VC, LaHue SC (2023) Reexamining cholinesterase inhibitors for the prevention and treatment of delirium in high-risk populations. Crit Care, 27: 129.
- Schlake K, Teller J, Hinken L, Laser H, Lichtinghagen R, et al. (2024) Butyrylcholinesterase activity in patients with postoperative delirium after cardiothoracic surgery or percutaneous valve replacement- an observational interdisciplinary cohort study. BMC Neurol. 24: 80.
- Brattinga B, Plas M, Spikman JM, Rutgers A, de Haan JJ, et al. (2022) The association between the inflammatory response following surgery and post-operative delirium in older oncological patients: a prospective cohort study. Age Ageing. 51: afab237.
- Xiao MZ, Liu CX, Zhou LG, Yang Y, Wang Y (2023) Postoperative delirium, neuroinflammation, and influencing factors of postoperative delirium: A review. Medicine (Baltimore). 102: e32991.
- Gabrielle E Mintz, Edward R Marcantonio, Jeremy D Walston, Simon T Dillon, Yoojin Jung, et al. (2024) Inflammatory Indices and Their Associations with Postoperative Delirium, The Journals of Gerontology: Series A, glae285.
- Murray C, Sanderson DJ, Barkus C, Deacon RM, Rawlins JN, Bannerman DM, Cunningham C (2012) Systemic inflammation induces acute working memory deficits in the primed brain: relevance for delirium. Neurobiol Aging. 33: 603-16.e3.

Tables at a glance
Figures at a glance