Analysis of Postural Ergonomic Stressors of Dentistry Professionals on Improved Patient Chair Design Using Rapid Upper Limb Kinematics
Received Date: April 06, 2024 Accepted Date: May 06, 2024 Published Date: May 09, 2024
doi: 10.17303/jber.2024.8.101
Citation: Ugwuanyi B. Uchenna, Egwuagu M. Onyekachi, Nwankwojike B. Nduka, Onah T. Okechukwu (2024) Analysis of Postural Ergonomic Stressors of Dentistry Professionals on Improved Patient Chair Design Using Rapid Upper Limb Kinematics. J Biomed Eng Res 7: 1-13
Abstract
Dental patient chair was remodeled with multi position articulation headrest and hydraulic energy transmission technology in a manually, but independently operated single working unit design to improve access and ergonomics. Analysis of postural ergonomic stressors of dentistry professionals on the device was performed in accordance with ISO 11226 standard using ergonomic valuation parameters of the upper limb. The throughput efficiency of root canal treatment, 3rd molar extraction, denture repair and scaling and polishing were 11.5%, 15.4%, 18.6% and 23.1% in that order, of total percentage of treatment time, 770 minutes. Flexion/right was dominant asymmetric posture for all parts of the upper limb and in all treatments, in which moderate flexion/right was more involved. Static posture became more prevalent among all valuation parameters on treatments selected than non-neutral posture. Moderate flexion/right and holding time SP≥ 30 seconds were components of non-neutral posture and static posture that were promoters of postural ergonomic stressors. It was established that head and neck were the primary ergonomic risk vulnerabilities during the treatments.
Keywords: Dentistry Professionals; Limb Kinematics; Dental Patient; Ergonomics; Upper Limb
Introduction
Dental unit chair is an indispensable medical device, specially designed to support a patient’s body that is undergoing dental procedure [1-3]. It supports a patient’s whole body, like a recliner, but articulated, so that dentist can recline patients to virtually any position. Sustenance of dentistry and quality oral care for patient, therefore, depends on ergonomic fitness. To achieve this, product manufacturers and researchers set their design objective on automation, which morphed the device to medium-to- high end medical asset, with consequent exorbitant cost and ever-reliance on electricity. The consequence is limited access to dental healthcare in our communities, even when WHO enlisted access to healthcare as SDG goal in 2030 [4]. World Bank had ranked Nigeria as the world’s worst country with regards to access to electricity in energy indices [5]. Nonetheless, widely reported epidemiological studies have indicated high prevalence of MSDs in different fields of dentistry [6,7]. Remodeling of dental chair is absolutely essential to combating MSDs. Introducing multi position articulation headrest and hydraulic technology, operated manually, but independently, is a significant milestone in office design within the context of physical ergonomics. Having developed the device, the ergonomic evaluation is worth undertaking.
Quite a number of ergonomic stressors were identified, including repetition, forceful exertion, vibration, noise, contact stress, prolonged static posture, awkward posture [8]. Prolonged static posture and non-neutral posture are typical postural stressors that are primarily machine-dependent. Postural stressors refer to work-related constrained posture that impose muscular load on a worker. In assessing the major risks factors of musculoskeletal disorders/ work related musculoskeletal disorders, ergonomic assessment tools/methods are employed. These include: New Ergonomic Posture Assessment (NERPA), loading on the upper Body Assessment (LUBA), Upper Limb Risk Assessment (ULRA), Rapid entire body assessment (REBA), OWAS and rapid upper limb assessment (RULA) are few of them. In all these methods, OWAS, REBA and RULA are most common technique in evaluating body postures and load [9,10]. These were identified by [11] as widely popular tools, usually supported by observational method for postural data collection. [12] avers that these tools are used in all continents and vast areas including manufacturing , textile, pharmaceutical industries and medicine.
Literature Survey on Rapid Upper Limb Analysis Studies
[13] studied the work hazards associated with those risk factors regarding work-related upper limb disorders by investigating ergonomic risk factors and their association with musculoskeletal disorders among 104 Indian dentists by using the RULA method. The study discovered that the average body posture of the subjects was characterized by neck flexion and twisting, shoulder abduction and excessive forward trunk bending. They established the connection between the action level and the increasing frequency with regard to the reported health disorders in the back, neck and shoulder region, thus, concluded that RULA is an appropriate method for evaluating body postures among dentists. The kinematic analysis with the CUELA system has already been used successfully in several dentist- orthodontist – based studies including [14-16]. The goal of this approach is to provide insights into those dentistry operations- based static activities during which these positions occur most frequently. [17] studied forced posture of neurology residents in daily routine on the ward in Germany with the system.
Materials and Method
Subjects
The study involved 9 (3f/6m) registered dentistry professionals, with average age of 46.2 ± 5.7 years, body height: 165.1 ± 35.2 cm and body mass: 82.5 ± 10.6kg. All subjects were right-handed with average work experience of 14.5 ± 5.9 years, in dental clinics, Federal college of dental technology and therapy, Enugu, under federal ministry of health. The dental professionals were all licensed with relevant regulatory agencies: Medical and dental council of Nigeria, Dental technology registration board of Nigeria and Dental therapy registration board of Nigeria and Radiology association of Nigeria. Further to this, dentists were selected based on their demonstrated attention to detail, manual dexterity, interpersonal skills, innovativeness and knowledge of dentistry, experience, visual and cognitive abilities.
As a record of validity, the participants declared status of functionally non-impairment or patient of musculoskeletal pains/disorders. The patients, 9(5f/4m), were selected using convenience sampling of those that displayed cases identified in Table 1, whose mean age was determined as 49.8 ± 15.3years, and were reported to be free from systemic diseases. Arrival rate of patients with indicated cases followed poison distribution, hence, convenient sampling. Some of the patients selected declined to participate in the trial and were promptly replaced. The improved patient chair design aimed at traditional and general-purpose utility, which can easily be configured with work setting of each dental operatory. This study was approved by Ethical committee, directorate of research and development, federal college of dental technology and therapy, Enugu. All participant signed the informed consent in advance
Measurement Systems
CUELA System: The CUELA measurement system (IFA; Sankt Augustin, Germany) is a motion capturing system approximately 3 kg in weight; and consists of accelerometers [ADXL 103/203] gyroscopes [muRata ENC-03R] for the head, arms, legs, back, and potentiometers [Contelect] for back torsion [18]. It is capable of kinematic reconstruction of the joint angle and portability in all planes, via flexible cables connected to sensors, making real time scanning of body segment with a frequency of 50Hz and an angular accuracy of 1° [19], possible to build a 3D avatar. This avatar computes the 3 D coordinates of all joints and the relevant joint angles, from where the algorithms calculate postures such as sitting, standing, or walking. Possible drift errors resulting from integration of the gyroscope values are compensated by continuous mixing with the accelerometer data so that no relevant drift errors occur with this approach [20]. The dentistry professionals wore an upper body vest under their clinical coats, with attached data storage unit of the posture system on the back. The sensor system, located at the upper thoracic spine area, measures torsion, lateral flexion, and flexion of the upper body, while flexible shaft that merges into a lower sensor box detects lumbar spine area. Extremities are provided with more sensors to measure flexion and extension movements. Cervical spine posture is monitored with a sensor supported with a headband and connected to the upper sensor box of the thoracic spine. The application in CUELA system synchronizes data to produce patterns of dentistry professionals: exodontists, orthodontists, periodontists, general dentists, prosthodontists, and endodontists. Thus, these movements are made visible in an angle–time diagram.
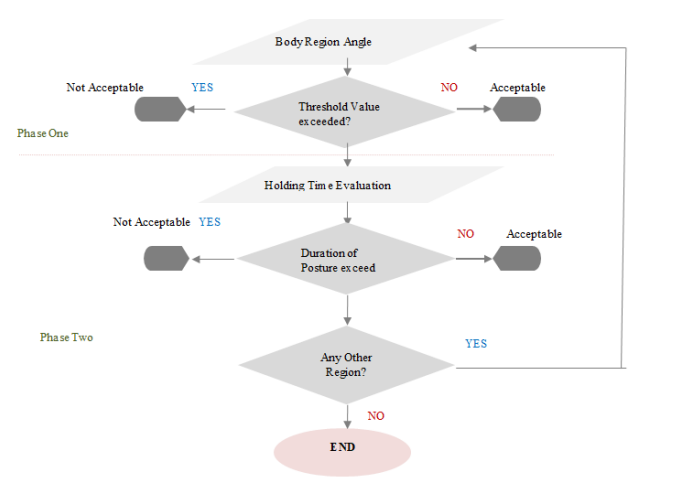
Data Evaluation: The computer-assisted acquisition and long term analysis of musculoskeletal loads (CUELA) system as a motion capturing system was inadequate of tracking all functional man-machine system for the professionals on the basis of product system analysis. Therefore the study was restricted to postural ergonomic stressors that were well captured in the system. In the context of the evaluation, activities are preselected based on their relevance and the percentage of the duration of the treatment of patients. The system is configuration was performed according to ISO 11226 ergonomic standard range [21] and program logic displayed on Figure1. The angle values of each body region (evaluation parameters) are assigned to a color-coded angle range in accordance with ergonomic standards by means of a traffic light system (red/yellow/green). Based on the respective colors, body postures are assessed as awkward, moderate or neutral [21-23]. Corresponding to this classification scheme, the percentage share of each evaluation parameter of the task is calculated and assessed as to whether it has been conducted in neutral, moderate or awkward body posture. Moderate and awkward body positions are added and summarized as non-neutral body postures. On this basis, the proportional static share of each evaluation parameter for the respective task is delineated as a further evaluation component. This portion of stasis (termed: total percentage of stasis) refers to static postures, are assessed according to ergonomic standards as moderate or awkward, and maintained for more than four seconds [21]. In practice, body postures can be maintained significantly longer than four seconds. The baseline static posture is 4s and further differentiation of ≥ 4 seconds, ≥ 10 seconds and ≥ 30s representing stasis components. Similarly, the postures are scaled as neutral, moderate and awkward moderate, according to ISO 11226 template. Consequently, the ratio of the total percentage stasis share and the percentage share of the total non-neutral postures are computed. This ratio represents the extent of the static percentage of the posture within the non-neutral postures identified as total percentage of stasis of non-neutral postures [16].
Mini- PC (Objective Activity Analysis): The objective activity analysis was established as a measurement method by Mache et al., in 2008, wherein the authors confirmed its validity and reliability for both inter- and intra –rater comparison [24]. Before the clinical, the work behaviors of the dentistry practitioners were documented through detailed and precise observations and analyses. The results were discussed and analyzed with heads of units involved (who were most experienced, and at grade level 13-15). Consequently, the activities were implemented into activity analysis software.in accordance with range of work, the computer program was well modified in advance and on the basis of detailed analyses so that all activities involved in standard operating practice were accommodated.
Experimental Procedure
The study did not involve all orofacial cases, but limited to a subset of nine treatments in the schedule of the institution clinics, drawn by the research team drawn and from cosmetic, preventive and restorative dentistry. Specific cases and stage(s) of treatments were brainstormed and collectively agreed on as in Table 1. The indicated procedures were allowed to complete their cycle, thence, not time- limited. Table 1 shows treatment template for the trial. The practitioners: exodontists, orthodontists, periodontists, general dentists, prosthodontists, and endodontists were appropriately kitted for the experimentation.
Results
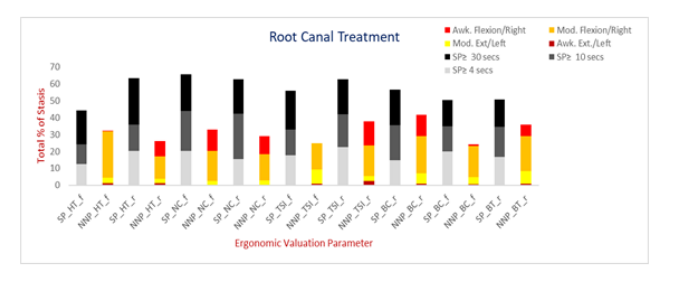
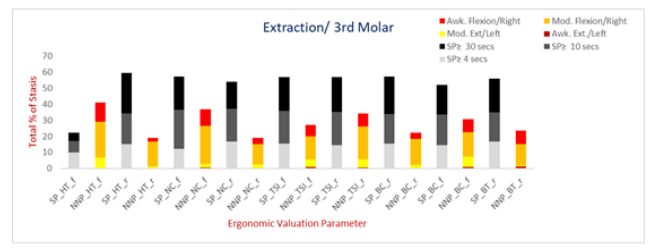
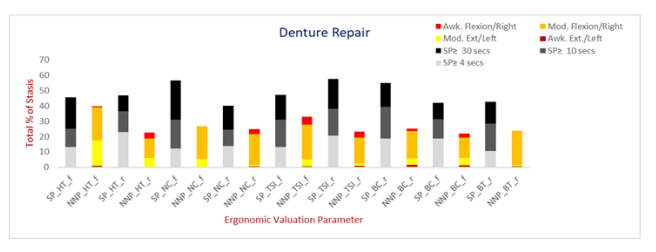
The kinematic data was obtained from UMPC, Samsung Q1, Samsung Electronics GmbH, Schwalbach, Germany portable computer during the experimentation . The data was extracted into Ms Excel for in-depth analytics and data visualization shown in Figure 2- 10.
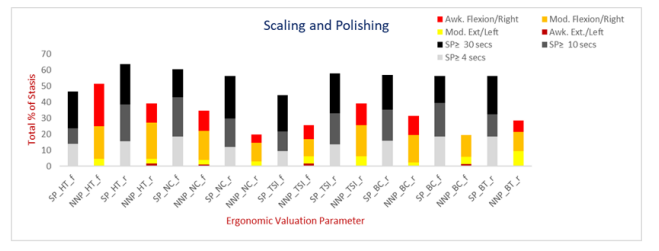
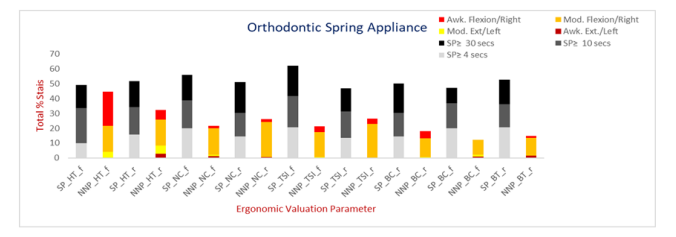
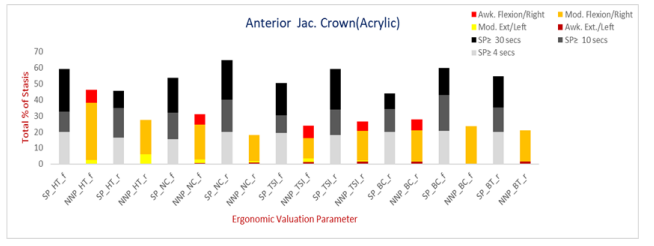
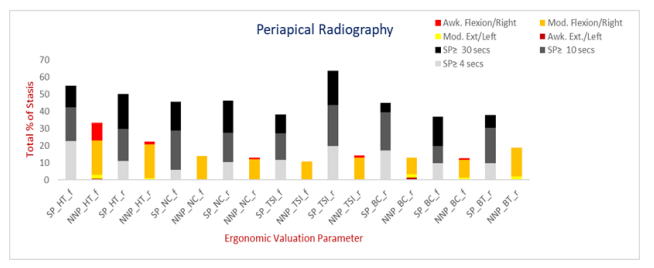
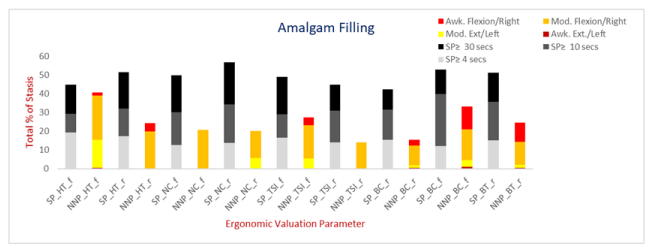
Figure 2 shows the total percentage of stasis of root canal treatment. In RCT, maximum muscular load occurred at neck. This part experienced percentage asymmetric flexion/extension posture of 35% of the time, which accounts for 32.6% flexion, including 14.6% of the time held in awkward posture. Figure 3 shows total percentage of stasis of 3rd molar extraction. At cervical part, 36.7% this proportion of time sustained compromised flexion/extension while 57% supported static posture. 25.9% of non-neutral posture time was held at moderate range and 10.8%, in awkward posture. Figure 4 shows total percentage of stasis of denture repairs. The neck sustained a load of 56.5% static posture and 26.7% non-neutral flexion. 26.6% of the nonneutral posture was within moderate range, which also comprise of 21.2% in flexion. Awkward posture was low at 0.1% of the time and occurred only in extension. At non neutral posture, holding time, SP≥ 30 seconds, was held for 25.4% of the regimen duration. Figure 5 shows total percentage of stasis of scaling and polishing(SP). Head experienced heaviest muscular load being held statically for 63.7% of the time, and 39.1% in asymmetric posture. In the lateral flexion, head tilt to right was dominant with 34.4% of the time, during which 22.4% was held in moderate range. Figure 6 shows total percentage of orthodontic spring appliance. During the procedure, head was supported in static posture of 48.9% of the time and 44.6% of extension/flexion. Flexion accounts for 40.3% of the time with a significantly high proportion of 22.9% held in awkward posture. However, there was no evidence of awkward extension in postural analysis. It was observed that the head was supported at 10.1% in SP≥ 4 seconds, 23.4% in SP≥ 10 seconds and 15.4% at SP ≥ 30 seconds. Figure 7 shows total percentage of teeth whitening. Muscular load during teeth whitening concentrated on the head. Static posture accounts for 55.4% of time and lateral flexion, 47.2%. 13.2% of the time was held static in SP≥ 4 seconds, 19.8% in SP≥ 10seconds and 22.4% in SP≥ 30seconds. Figure 8 shows total percentage of anterior jacket crown. The head supported maximum muscular load, being held statically for 59% of time. Of this, percentage holding time of SP≥ 4 seconds, SP≥ 10 seconds and SP≥ 30 seconds were 19.9%, 12.8% and 26.3% respectively were recorded. In addition, extension/flexion of the head was maintained for 46.1% of the time, with 43.7% locked in flexion. Figure 9 shows total percentage of stasis of Periapical radiography. The head was held statically for 54.8% treatment time in extension/flexion posture, while asymmetrical posture was maintained for 33.4% of regimen duration. This consisted of 30.3% flexion, including 19.8% held within moderate range and 10.5% in awkward posture. Figure 10 shows total percentage of stasis of amalgam filling. Extension/flexion of torso was maintained for 33.1% and held statically for 52.9%. Of this non neutral posture, 28.3% occurred in flexion, including 16.3% held in moderate range.
Discussions
In a global view, flexion/right was dominant asymmetric posture for all parts of the upper limb and in all treatments. Moderate flexion/right was more involved in the treatments. This trend bears similitude to [17] study involving forced posture of neurology residents on non-clinical activities. Static posture became more prevalent among all valuation parameters on treatments selected, with SP≥ 30 recording significant higher proportion. This holding time sustained in asymmetric posture represents postural stressors. Head and neck recorded the maximum non-neutral posture for the selected treatments, certe, awkward and moderate flexion/right.
On treatment –to- treatment basis, head and torso were held in flexion mostly at SP≥ 30 seconds, while lateral flexion was sustained most at neck, thoracic spine and torso, during anterior jacket crown treatment. The increased holding time is attributable to attention to details on chipped incisor, producing a cumulative load on the head and neck. The head assumes a kyphotic posture, where the neck is extended corresponding to the total percentage of non-neutral posture, in an inflicted position of the head and entire back. This is in agreement with [25] that prosthodontics have 80% prevalence of MSDs, occurring at neck. In orthodontic spring appliance procedure, the head and thoracic spine were held in flexion, mostly at SP≥ 10 seconds. Lateral flexion recorded peak non-neutral posture, being held mostly moderately, at head and neck. The compromised posture is partly due to lingual bracing with forsus springs. This corroborates [14,15] that the greater angle values of head and cervical spine area of dentist and orthodontist showed that treatment activities were increasingly conducted in forced postures. According to [26], orthodontists experience pains due to forward positioning of head and bending of lower back during clinical procedures. Denture repairs experienced most static posture maintained for SP≥ 4seconds at head, neck and torso. The most asymmetric posture was recorded on moderate flexion of thoracic spine. The data shows improved stasis on most parts of upper limb. Extraction of 3rd molar shows an enormous load on the neck and thoracic spine is a resultant effect of sustaining force load at 23.6% of non-neutral posture moderately, while statically held SP≥ 10 seconds for 24.5% of static posture. When this circumstance is considered for 18.6% of the total time of treatment regimen, and other possible ergonomic stressors, 3rd molar extraction has profound indication for musculoskeletal disorder. The finding is consistent with epidemiological studies of [7,27], who concluded that neck and shoulder parts have highest prevalence of MSDs, and occur more among orthodontists, oral physicians, general practitioners and hygienists. Amalgam filling forced torso statically in flexion for SP≥ 10 seconds in 27.5% of static posture. During the treatment, torso, and thoracic spine were held more in moderate posture. This could have great influence on the development of biomechanical effect, but is negligible due to low proportion of treatment time (3.2%). Root canal treatment recorded poor stasis in all parts of upper limb. The neck and thoracic spine, indicated incidences of heaviest muscular load, which were held statically in flexion at SP≥ 10 seconds, while maintaining lateral flexion/right mostly at SP≥ 10seconds. This posture is maintained for 23.1% of the total time of treatment, the longest duration of treatment time. [26] avers that general practitioners are more predisposed to neck and low back MSDs as a result of prolonged static posture and fewer repetitive motions.
Scaling and polishing procedure was sustained by neck and torso statically at SP≥ 10 seconds, in flexion for at least 20.8% of static posture. The parts maintained lateral flexion /right, in static posture of SP≥ 30 seconds by head and torso. Specifically, the head maintained an awkward posture of 26.4% of 46.7% in flexion and neck sustained 18% of 30.5% in moderate flexion. The distribution of muscular load corroborates [26] work that dental hygienists and periodontists have neck, shoulder and wrist MSDs due to static posture, forceful and repetitive movements adopted during procedure. The stasis is, even, exacerbated in high operational demand in manual scaling of heavy mouth (term that expresses large amount of calculus). [28] identified these prolonged static postures and non-neutral posture, in addition to repetitive motion and mechanical force as primary factors of aetiology of MSDs that imperil job demands of hygienists. Teeth whitening are a cosmetic dentistry procedure aims at improving aesthetics of patients. Only the head part of upper limb experienced 20.5% static posture of SP≥ 30 seconds, held in flexion. The head and neck were found to be held at moderate flexion. In periapical radiography, there was general decline in stasis, as a result of machine performing examinations with little human intervention. However, lateral flexion/ right of thoracic spine was most affected degree of freedom, which occurred during preparation of patient for radiography. It can be seen from the data that total percentage of stasis of static posture of 23.8% was held statically for SP≥ 10 seconds, maintained for 5.6% of the total time of treatment. Although classified as forced posture, it is not viewed seriously, as long as it is not performed permanently
Considering total percentage of treatment time of scaling and polishing, denture repairs, 3rd molar extraction and root canal treatment that recorded 11.5%, 15.4%, 18.6% and 23.1% in that order, of 770 minutes and carrier-long practice, the aetiology of musculoskeletal disorders (MSDs) become obvious. These are medically identified as kyphosis, scoliosis, lardoses, cervical spondylitis, lumbar radiculopathy, trapezium myalgia among others [31]. It could be established that head and neck were the primary targets of muscular load during the treatments. Nonetheless,[32] using the RULA method, stated that increased potential risk from static posture of more than 30sec is mainly referred to the thoracic spine and back area. These results are not exclusive of dental chair only but combination of complexity of selected cases, low level of instrumentation and orthogonathic anatomy of jaw. However, previous studies were bereft of detailed analysis, the discussions correlate with performance of improved design. But the actual performance could of the device can only be drawn from calibration of the device.
It is noteworthy to state ergonomic interventions in dental practice to mitigate these stressors. Typically, activity change and frequent interruptions were well noticed and essential component that relieve and recover spinal stability intermittently. Alternate work positions between sitting and standing, intermittent body, neck and back stretching exercises as well as shoulder release [29,30] are essential remediation to musculoskeletal disorders. Stretch increase blood flow to muscles, increase production of synovial joint fluid, and create a relaxation response and identifying ‘tight’ muscles that may be predisposed to pain, injury or a career-ending musculoskeletal disorders in dentistry.
Conclusion
The treatments were provided by right-handed dentistry professionals. Scaling and polishing, denture repairs, 3rd molar extraction and root canal treatment were observed to have low throughput efficiency. Static posture became more prevalent among all valuation parameters on treatments selected than non-neutral posture. In granularity, moderate flexion/right and holding time SP ≥ 30 seconds were components of non-neutral posture and static posture that were promoters of postural ergonomic stressors. It was established that head and neck were the primary targets of muscular load during the treatments. With the experimentation, it is evident that the medical device could be deployed off-grid, and represents an improvement in access, but impact of multi position articulation on ergonomics can only be ascertained after calibration of the device.
Ethical Approval
Ethical clearance was obtained from Director of research and development, on behalf of ethical committee, Federal College of Dental Technology and Therapy (now Federal University of Allied Health Sciences) Enugu, for experiments in dental clinics.
Acknowledgements
The completion of the research would not have been possible without contribution of individuals and organisations. My mentors Engr Prof. B.N. Nwankwojike, Dr O.M. Egwuagu, and Dr T.O. Onah made invaluable input throughout the research. Managements of Scientific Equipment Development Institute, Akwuke, Federal College of Dental Technology and Therapy, Enugu and Enugu State University of Science and Technology are gratefully acknowledged.
- HR Fajrin, KM Husodo K. Supriyadi (2020) Dental unit prototype with electric dental chair and dental light parameters” in 2020 Proceedings of the 4th international conference on sustainable innovation , Technology, Engineering and Agriculture (ICoSITEA 2020), 199.
- IM Fikriah, V Asfirizal, C Bhakti, MP Ikbal (2020) Design simulator dental unit for practice of dental medicine student, European Journal of Clinical Medicine, 7: 694-70.
- M Foutse, M Youssoufa, PT Kapen, SCTchounang (2020) Low-cost mobile dental unit for oral care service delivery in third world countries: From concept to operation, Health Technology, 10: 1525-32.
- World Bank (2021) Tracking SDG 7: The energy progress report (2021). International renewable energy agency, World Bank data.
- World Bank (2022) Nigeria has world’s largest electricity access deficit.
- D Ohlendorf, A Naser, Y Haas, J Haenel, L Fraeulin, et al. (2020) Prevalence of musculoskeletal skeletal disorders among dentists and dental students in Germany, International Journal of Environmental Research and Public Health, 17: 8740.
- J Lietz, A Kozak, A Nienhaus (2018) “Prevalence and occupational risk factors of musculoskeletal diseases and pain among dental professionals in western countries: a systematic literature review and meta-analysis, PLoS ONE, 13.
- A Gupta, M Bhat, T Mohammed, N Banal, G Gupta (2014) Ergonomics in dentistry, International Journal of Clinical Pediatric Dentistry, 7: 30-4.
- D Kee (2020) Systematic comparison of OWAS, RULA and REBA based on literature review, International Journal of Environmental Research and Public Health, 19: 595.
- D. Roman-Liu (2014) Comparison of concepts in easy-to-use methods of MSD risk assessment, Applied Ergonomics, 45: 420-7.
- M Josh, V Deshpande (2022) Study of association between OWAS, REBA and RULA with perceived exertion rating for establishing applicability, Theoretical Issues on Ergonomics Science, 23: 313-32.
- TS Ogendengbe, AO Abiola, MI Omolayo, SA Adeniran, IM Adekunle, OA Abiola, et al. (2022) Ergonomics postural risk assessment and observational techniques in the 21st century, Proceedings in Computer Science, 217: 1335-44.
- V Golchha, P Sharma, J Wadhwa, D Yadav, R Paul, (2014) Ergonomic risk factors and their association with musculoskeletal disorders among Indian dentist: a preliminary study using rapid upper limb assessment, Indian Journal Dentistry Research, 25: 767-71.
- D Ohlendorf, C Erbe, I Hauck, J Nowak, I Hermanns, D Ditchen, et al. (2016) Kinematic analysis of workrelated musculoskeletal loading of trunk among dentists in Germany, BMC Musculoskeletal Disorder, 17: 427.
- J Nowak, C Erbe, I Hauck, DA Groneberg, I Hermanns, R Ellegast, et al. (2016) Motion analysis in the field of dentistry: a kinematic comparison of dentists and orthodontists, BMJ Open, 6: e011559.
- D Ohlendorf, C Erbe, J Nowak, I Hauck, I Hermanns, D Ditchen, et al. (2017) Constrained posture in dentistry- a kinematic analysis of dentists, BMC Musculoskeletal. Disorders, 18: 1-15.
- A Bijanzadeh, H Ingo, R Ellegast, L Fraeulin, F Holzgreve, et al. (2021) Forced posture in neurology residents in daily routine on the ward in Germany, Manuelle Medizin, 59: 269-82.
- RP Ellegast (1988) Person-mounted measuring system for automated recording of loads on the spinal column during occupational activities, HVBG, Sankt Augustin.
- S Freitag, R Seddouki, M Dulon, JF Kersten, TJ Larsson, A Nienhaus (2014) The effect of working position on trunk posture and exertion for routine nursing tasks: An experimental study, Annual Occupational Hygiene, 58: 317-25.
- I Hermanns, N Raffler, S Fischer, B Gores, R Ellagast (2008) Simultaneous field measuring method of vibration and body posture for assessment of seated occupational driving tasks, Int Z Arbeitsergonomie 38: 255-63.
- ISO 11226 (2000) Ergonomics-evaluation of static working postures, International organization for standardization, Geneva Switzerland: International Organization for Standardisation.
- DIN EN 1005–1 (2002) Sicherheit von Maschinen-- Menschliche körperliche Leistung-Teil, 1: Begriffe Berlin: Beuth Verlag GmbH.
- DIN EN 1005–2 (2003) Sicherheit von Maschinen Teil 2: Menschliche körperliche Leistung; Manuelle Handhabung von Gegenständen in Verbindung mit Maschinen und Maschinenteilen, Deutsche Fassung EN 1005–2:2003. Berlin: Beuth Verlag GmbH.
- S Mache, C Scutaru, K Vitzthum, A Gerber, D Quarcoo, T Welte, et al. (2008) Development and evaluation of a computer-based medical work assessment programme, Journal of Occupational and Medical Toxicology, 3: 35.
- C Batham, Y Sandul (2016) A risk assessment study on work-related musculoskeletal disorders among dentists in Bhopal, India, Indian Journal of Dentistry Research, 27: 236-41.
- B Valachi, K Valachi (2003) Mechanisms leading to musculoskeletal disorders in dentistry, Journal of American Dental Association, 134: 1344-50.
- D Ohlendorf, A Naser, Y Haas, J Haenel, L Fraeulin, C Holzgrave, et al. (2020) Prevalence of musculoskeletal skeletal disorders among dentists and dental students in Germany, International Journal of Environmental Research and Public Health, 17: 8740.
- H Das, V Mortghare, M Singh, (2018) Ergonomics in dentistry: Narrative review, International Journal of Applied Dentistry Science, 4: 104-10.
- A Gupta, M Bhat, T Mohammed, N Banal, G Gupta (2014) Ergonomics in dentistry, International of Clinical Pediatric Dentistry, 7: 30-4.
- D Garewal, JK Chawla, S Sharma, (2016) Ergonomics solutions in dental practice, Journal of Medical Science and Clinical Research.
- L Lui, B Chung (2022) Common musculoskeletal injuries in dental practice.
- HS Park, J Kim, HL Roh, S Namkoong (2015) Analysis of the risk factors of musculoskeletal disease among dentists induced by work posture, Journal of Physical Therapy Science, 27: 3651-4.


Tables at a glance
Figures at a glance