Emergency Transcatheter Aortic Valve Implantation in A Patient with The Assistance of Intra-Aortic Balloon Pump
Received Date: October 20, 2021 Accepted Date: November 20, 2021 Published Date: November 22, 2021
doi: 10.17303/croa.2021.6.202
Citation:Yan Xu (2021) Emergency Transcatheter Aortic Valve Implantation in A Patient with The Assistance of Intra-Aortic Balloon Pump. Case Reports: Open Access 6: 1-6.
Abstract
Surgical aortic valve replacement (SAVR) is considered the gold-standard treatment for patients with severe aortic valve stenosis (AS), yet 30% are considered inappropriate for SAVR on account of the advanced age and multiple comorbidities. Transcatheter aortic valve implantation (TAVI) provides an option for high-risk patients with severe AS, especially for those accompanied with acute cardiogenic shock and multiple organ dysfunction. Herein, we presented a case of a patient resuscitated successfully with TAVI in combination with intra-aortic balloon pump IABP.
Keywords:Aortic Valve Stenosis; Cardiogenic Shock; Transcatheter Aortic Valve Implantation; Intra-Aortic Balloon Pump
Case Report
Aortic valve stenosis (AS) is the most common valvular disease in the Western world, especially among individuals above 60 years of age [1]. It is associated with a high rate of death if untreated. Surgical aortic valve replacement (SAVR) is considered the gold-standard treatment for patients suffering from severe AS. However, SAVR is not feasible in approximately 30% of the patients, due to advanced age and multiple comorbidities [2]. Complications such as cardiogenic shock and multiple organ dysfunction syndrome (MODS) pose a great challenge to SAVR, and lead to an operative mortality as high as 21% [3]. Recently, interventional therapy such as transcatheter aortic valve implantation (TAVI) has provided an alternative option for these high-risk patients, [4-6] yet the feasibility for treating severe AS patients with cardiogenic shock and MODS has not been established. Herein, we presented an extremely severe AS case complicated with acute cardiogenic shock and MODS who successfully saved by emergency TAVI with the assistance of intra-aortic balloon pump (IABP). Written consent was received from the patient for publication of this case report.
Case presentation
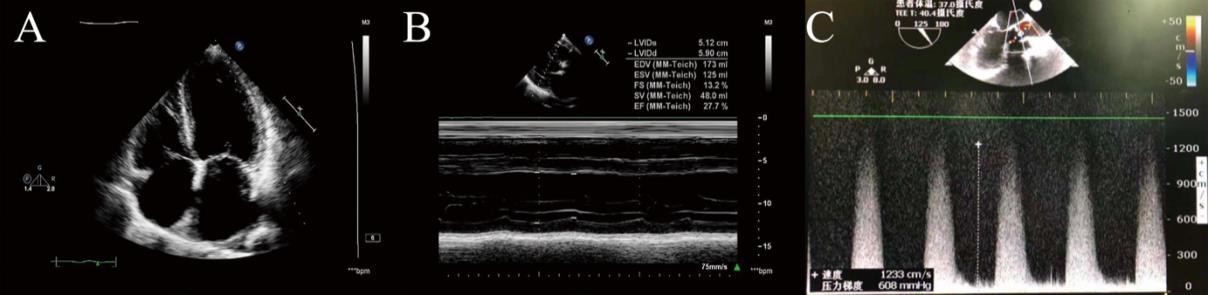
A 74-year-old male patient presented to the emergency department with progressive shortness of breath for several months. He also reported a harsh cough with occasional purulent sputum production. He had a history of AS, hypertension and coronary artery disease. His AS and coronary artery disease were treated with conservative treatment. Physical examination revealed a 5/6 systolic murmur in aortic area and bilateral lower extremity edema. Transthoracic echocardiography (TTE) and Transesophageal echocardiogram (TEE) demonstrated an extremely severe AS with the aortic valve area (AVA) of 0.5 cm2, peak AV velocity of 12.33 m/s, peak transaortic pressure gradient (PG) of 608 mmHg, a significantly decreased left ventricular ejection fraction (LVEF) of 27.7%, mild
mitral regurgitation as well as tricuspid regurgitation (Figure 1).
His condition deteriorated rapidly with conservative management. Acute cardiogenic shock, renal failure and respiratory failure developed after he was admitted to the cardiovascular surgical unit. His vital signs were as follows: heart rate (HR) 111bpm, blood pressure (BP) 75/33 mm Hg, respiratory rate (RR) 24 bpm, and saturation of pulse oxygen (SpO2) 70%-80% when given a reservoir bag mask of 6 L/min. Laboratory tests revealed BNP >35000 pg/ml, urea 28 mmol/l, serum creatinine 175.0 μmol/l, AST 2373 IU/L, ALT 1788 IU/L, TB 131.7 μmol/l and DB 90.4 μmol/l. Arterial blood gas test showed pH 7.288, PCO2 53 mmHg, PO2 67 mmHg and BE -6.96 mmol/l. The patient was transferred to the cardiac intensive care unit (CCU) after tracheal intubation. As his conditions deteriorated, IABP was placed to improve coronary perfusion pressure in CCU.
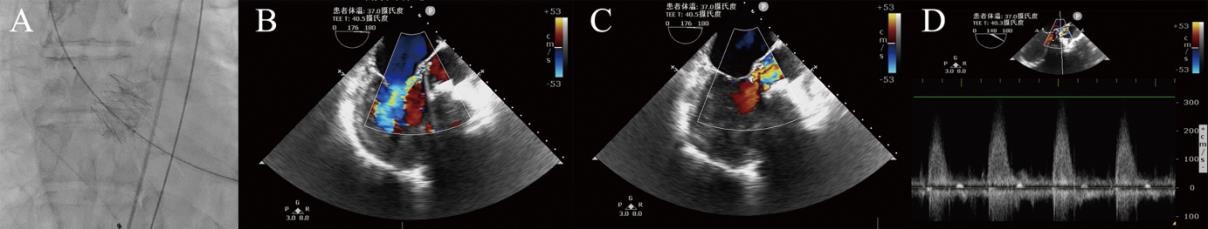
The patient was then scheduled for TAVI with the assistance of IABP and high dose of epinephrine and norepinephrine. In the hybrid operating room (OR), his baseline HR was 109 bpm, BP was 80/40 mmHg, and SpO2 (FiO2 50%) was 92%. General anesthesia was induced
with 2 mg midazolam, 20 μg sufentanyl and 50 mg rocuronium, and then maintained with 1-1.5% sevoflurane. A 25-mm SAPIEN transcatheter heart valve (Ed- wards Lifesciences) was deployed successfully through a transapical approach with the guidance of cinefluoroscopic and TEE. (Figure 2). Immediately after deployment of the valve, the patient demonstrated significant hemodynamic improvement and the peak AV velocity dropped from 12.33m/s to 3.2m/s, with epinephrine reduced from 0.3 to 0.1μg/kg/min and norepinephrine was reduced from 0.8 to 0.3 μg/kg/min iv. The surgery lasted 120 minutes, and the whole procedure was smooth and uneventful. IABP was used intraoperatively to assist circulation.
No adverse cardiac events, e.g, cardiac arrest or malignant arrhythmia, occurred in the OR.
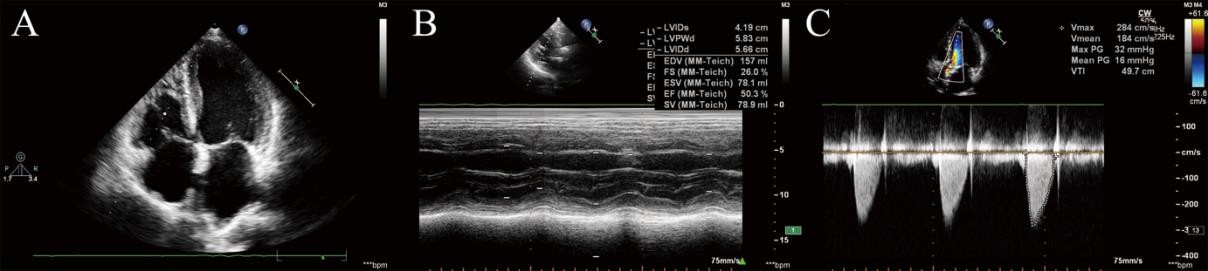
The patient was then transferred to CCU and carefully weaned off catecholamines. He was extubated two days later when BNP decreasing to 4667 pg/m. The IABP was removed on the fourth postoperative day. Simultaneously, renal and respiratory function was gradually improved. The patient was discharged from hospital 11 days after surgery without any complications. In the six-month follow-up, the patient’s cardiac function was improving from NYHA class IV to II. Additionally, the TTE showed the mean transvalvular gradient and AVA were 16 mmHg and 1.4 cm2 respectively, and LVEF increased to 48% without any inotropic agents support (Figure 3).
Discussion
Severe AS with acute cardiogenic shock and MODS are lethal and require prompt treatment [7-8]. SAVR remains the first choice in younger or lower risk AS patients, yet critically ill elderly patients are at high-risk for SAVR [9]. Therefore, TAVI has been increasingly recommended for the avoidance of cardiopulmonary bypass, traditional sternotomy and cardioplegia [9]. Nevertheless, the feasibility of TAVI for treating severe AS patients with acute cardiogenic shock and MODS has not been established. In this article, we presented an extremely severe AS case with above complications, successfully resuscitated emergency TAVI under the assistant of IABP.
In our case, the patient was admitted with cardiogenic shock and MODS. Following short-term conservative medical management, his condition continued to deteriorate. Then, IABP was employed to enhanced myocardial perfusion and support circulation as a bridging therapy to TAVI. IABP is inflated during diastole to enhanced myocardial perfusion, and deflated during systole to reduce cardiac afterload. Moreover, IABP placement also permitted reduction in vasopressor requirements [10]. Although using IABP in combination with VA-ECMO is a reasonable strategy for cardiogenic shock, the effectiveness of this combination remains controversial in patients with limited survival and is occasionally criticized for its high cost. Thus, ECMO was not applied due to its specific complications (cardiac thrombosis and the coronary or cerebral hypoxia) and high cost in this case. Notably, the anesthetist played a critical role during the whole procedure. The anesthetist must be prepared to treat any sudden arrhythmias such as ventricular fibrillation or atrioventricular block, as a result of rapid ventricular pacing or manipulation of catheters within the heart. In this case, general anesthesia was used because it allows control of the procedure with a secure airway in completely immobile patient [11]. More importantly, general anesthesia allows the use of transesophageal echocardiography, which can provide important information perioperatively. In addition, a “titrate to effect” induction method is necessary, and the anesthetics that do not rely on renal and liver function are better choice. Hypotension should be treated aggressively with vasoactive agents, followed by management of the underlying cause. The main goal of intraoperative management is to protect the failing heart and organ by optimizing oxygen supply and decreasing oxygen demand, and excessive fluid infusion should be avoided except for unexpected massive bleeding. With the meticulous anesthetic management and IABP support, the whole TAVI procedure was smooth and uneventful.
In summary, TAVI is a realistic life-saving option for these patients with severe AS and cardiogenic shock who would otherwise encounter death. The development of TAVI has allowed successful treatment for patients who were previously deemed too risky for SAVR, and bridging therapies such as IABP and vasopressors are important supplement treatments. However, effects of TAVI remain to be established in such high-risk patients on long-term outcome.
Funding
This work was supported by the Sichuan University Huaxi Hospital Discipline Excellence Development 1.3.5 Project (2018HXFH046) and the Sichuan Provincial Scientific Grant (2017SZ0110).
- Iung BA (2003) prospective survey of patients with valvular heart disease in Europe: The Euro Heart Survey on Valvular Heart Disease. Eur Heart J 24: 1231-43.
- Nkomo VT, Gardin JM, Skelton TN (2006) Burden of valvular heart diseases: a population-based study. The Lancet 368: 1005-11.
- Carabello BA, Green LH, Grossman W (1980) Hemodynamic determinants of prognosis of aortic valve replacement in critical aortic stenosis and advanced congestive heart failure 62: 42-8.
- Craig RS, Martin BL, Michael JM (2011) Transcatheter versus Surgical Aortic-Valve Replacement in High-Risk Patients. N Engl J Med 364: 2187-98.
- Haude M (2017) Management of valvular heart disease: ESC/EACTS guidelines Herz 42: 715-20.
- Liu Z, Kidney E, Bem D (2018) Transcatheter aortic valve implantation for aortic stenosis in high surgical risk patients: A systematic review and meta-analysis. PLoS One 13 : e0196877.
- Rosenhek R, Binder T, Porenta G, (2001) Predictors of Outcome in Severe, Asymptomatic Aortic Stenosis. 10: 75.
- Carabello BA, Paulus WJ (2009) Aortic stenosis. The Lancet 373: 956-66.
- Schmidt T, Frerker C (2019) Treatment Challenges in Patients with Acute Heart Failure and Severe Aortic Valve Stenosis. Curr Cardiol Rep 21: 47.
- Almufti F, Morris N, Lahiri S, et al. (2016) Use of Intra-aortic- Balloon Pump Counterpulsation in Patients with Symptomatic Vasospasm Following Subarachnoid Hemorrhage and Neurogenic Stress Cardiomyopathy 9: 28.
- Welt FG, Davidson MJ, Leon MB (2011) Transcatheter aortic valve replacement. Circulation 124: 2944-8.

Figures at a glance