I Need to Dialysis, I Can’t Breathe!
Received Date: September 26, 2021 Accepted Date: October 26, 2021 Published Date: October 28, 2021
doi: 10.17303/croa.2021.6.201
Citation:Torrens Jonathan (2021) I Need to Dialysis, I Can’t Breathe!. Case Reports: Open Access 6: 1-4.
Abstract
One of the advantages that science has brought to medicine is renal replacement therapy. With the evolution of medicine, different types of therapy have been developed; and many patients can choose the type that best fits with their lifestyle. However, risk and complications could affect the availability of renal replacement therapy for each patient. Since 1913, there are descriptions of how to filter the blood as a healthy kidney will do. The main purpose of renal replacement therapy is to remove solute using the forces of diffusion, coveccion and filtratrion. Different modalities has been described in the literature using extracorporeal and paracorporeal methods. Extracorporeal refers to use of artificial tubes and membranes where blood is pass though for dialysis. Paracorporeal use the peritoneal membrane for exchange of solutes and fluid. Patients has to be evaluated and educated on the process of peritoneal dialysis, before starting the therapy due to catheter care and cyclers use. Dyalize is injected by the patient manually or by autonomous cycler in the peritoneal area and dwell for a stablish time.
Keywords:Pleuro-Peritoneal Leak; Pleural Effusion; Pleural Disease
Case Report
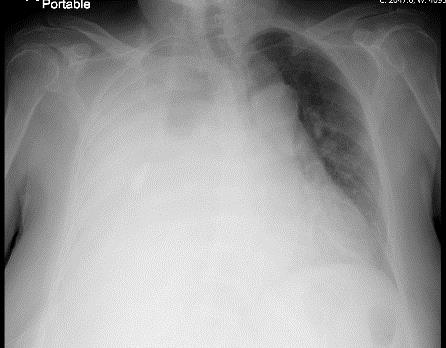
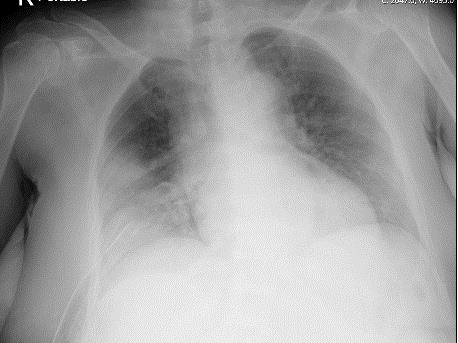
This is the case of a 63 y/o female patient, with a past medical history of adult polycystic kidney disease (ADPKD), hypertension, hypothyroidism, and hypercholesterolemia that was started on peritoneal dialysis one month ago. Patient presented to emergency department with shortness of breath and fatigue for the past 3 weeks that was getting worse, causing fatigue and orthopnea. Physical examination was remarkable for decreased breath sounds on the right side, no jugular venous distention, no peripheral edema, and patent peritoneal dialysis tunneled catheter in the abdomen. Portable chest x-ray reported diffuse right white lung with mass-effect towards the left. The Chest CT scan without IV contrast reported large right-sided pleural fluid collection with near total collapse of the lung and polycystic kidney disease. Due to large amount pleural fluid, surgery services were consulted for chest tube placement. The analysis result of the pleural fluid was consistent with transudate fluid and elevated glucose level (69 mg/dl). She had relief after chest tube drainage and no recurrence of pleural effusion occurred after patient was switched to hemodialysis. Findings suggest a pleuroperitoneal leak, due to given history of ADPKD with pleural effusion that occurs early after peritoneal dialysis initiation, and no other clinical findings of fluid overload.
Discussion
Pleuroperitoneal leak is a rare complication of peritoneal dialysis with an incidence of 1.6% to 10%, where women are more affected. This condition may occur due to communications between the pleura and the peritoneum. In addition, patients with ADPKD are predisposed to develop this non-infectious complication due to increased hydrostatic pressure. However, many occasions pleural effusion resolve with overnight dwells. Our patient required chest tube placement for resolution of symptoms, and she could not be a candidate to continue with peritoneal dialysis. Although, if patient were aware of her predisposition and seek medical attention earlier conservative measures could be implanted and patient may continue with her current mode of therapy. This case serves for remainder about the importance of educating patient about how to identify therapy complications.
- Fleming GM (2011) Renal replacement therapy review: past, present and future. Organogenesis, 7: 2–12.


Figures at a glance