A Rare Anatomical Variant Causing a Common Respiratory Complain
Received Date: September 10, 2022 Accepted Date: October 10, 2022 Published Date: October 14, 2022
doi: 10.17303/croa.2022.7.103
Citation: Padilla Rodriguez KC, Jonathan Torrens Olan, Ivanisse Ortiz Velez, Juan Gracia Puebla, Ricardo Fernandez Gonzalez (2022) A Rare Anatomical Variant Causing a Common Respiratory Complain. Case Reports: Open Access 7:1-4
Abstract
Chronic cough is defined as a cough lasting for more than 8 weeks and roughly 80% can be attributed to gastroesophageal reflux disease, allergic rhinitis and asthma.
Keywords: Tracheobronchopathia osteochondroplastica; chronic cough; unexplained cough; bronchoscopy
Introduction
Cough is certainly one of the most common symptoms encountered by clinicians. Usually it is self-resolving, yet in some instances it may be secondary to a bothersome chronic condition. Chronic cough is defined as a cough lasting for more than 8 weeks and roughly 80% can be attributed to gastroesophageal reflux disease, allergic rhinitis and asthma [1]. Other more uncommon causes should be suspected when diagnostic tests and treatment have excluded ordinary causes. Tracheobronchopathia osteochondroplastica (TO) is a rare benign disorder affecting the tracheobronchial tree in which 54% of the patients experience chronic cough.
Case Presentation
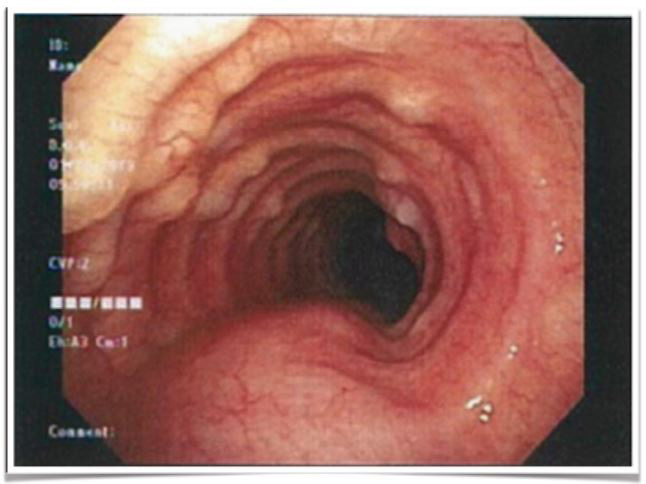
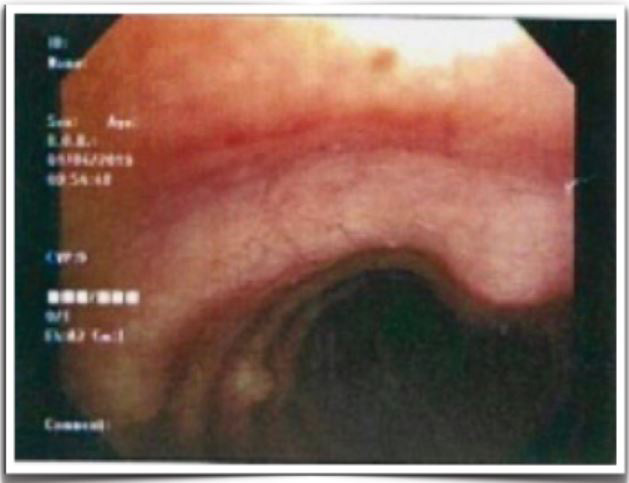
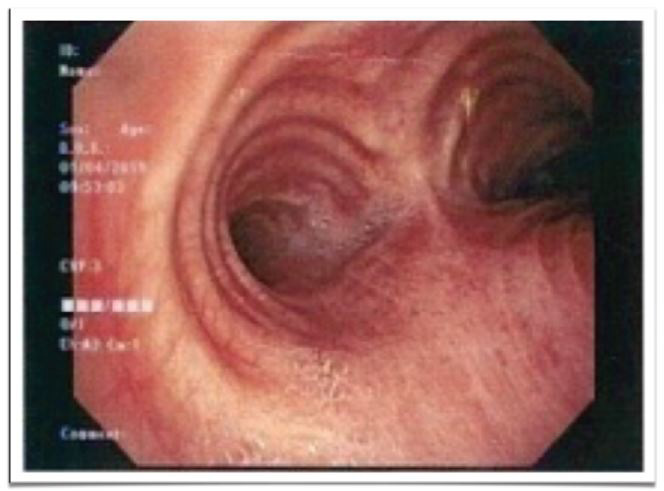
A 70 year old female with prior history of hypothyroidism, gastroesophageal reflux disease, allergic rhinitis and mild intermittent asthma complaining of a nonproductive cough of more than three years evolution. She also reported occasional hoarseness and clearing of the throat. Treatment including proton pump inhibitors, intranasal steroids, antihistamines, benzonatate, leukotriene inhibitors, inhaled and oral steroids failed to resolve her complaints. Physical examination was essentially normal. Vital signs stable with adequate parameters. Pulmonary function test was unremarkable. Diagnostic imaging demonstrated multiple subtle tracheal polyps reason why a flexible bronchoscopy was performed. Findings were consistent of multiple nodular projections in the anterior and lateral aspects of the trachea. These nodules were present only above the tracheal cartilaginous rings [figures 1-3]. Given the characteristic appearance and distribution of these nodules the diagnosis of TO was made. Treatment is not often done unless cases of severe airway obstruction where resection or laser may be required [3]. In this case, patient did not present with airway obstruction and was managed with conservative treatment.
Discussion
TO is a rare disorder of unknown cause in which numerous sessile, cartilaginous or bony nodules project into the airway lumen from the anterolateral walls of the trachea. Often under diagnosed and mislabeled, estimated incidence ranges between 0.4% - 0.8% during bronchoscopic evaluation. Overall prevalence ranges from 0.01 to 4.2 per 100,000 patients [2]. Unlike our case, this disorder is more common in men and the diagnosis is usually made in the fourth through sixth decades of life [5]. This condition remains essentially untreatable in the absence of airway obstruction and thus symptom management is most often the norm, although sometimes invasive procedures are necessary. Antibiotics are used to treat respiratory tract infections, antitussives and inhaled corticosteroids are used to treat cough [6]. If obstruction is present, mechanical measures to remove obstruction nodules are done either by cryotherapy, laser excision, external beam irradiation, radiotherapy, stent insertion or surgical resection therapy [7]. Differential diagnosis include amyloidosis, relapsing polychondritis, sarcoidosis, tuberculoid calcifications, dermatomyositis, scleroderma, Wegener's granulomatosis and tracheal polyposis. Chronic cough may feel like a burden affecting patients mentally and physically impacting significantly their quality of life. This case should prompt clinicians to always include TO in the differential diagnosis of chronic cough and raise awareness towards the importance of bronchoscopic evaluation in patients with unexplained persistent cough.
Conclusion
Frequent causes of chronic cough are gastroesophageal reflux disease, allergic rhinitis and asthma. If unexplained persistent cough continues despite treatment of common causes, further studies should be considered including a bronchoscopic evaluation. Pulmonary function testing generally does not show airflow limitation. Only a small fraction of patients have ventilation anomalies, most commonly bronchial obstruction [6]. Tracheobroncopathia Osteochondroplasica are bening nodularities that protrude toward the lumen of the large airway [3]. Nodularities may vary in size from suttle to obstructive and may present as chronic cough. The bronchoscopic appearance alone is diagnostic of the disease, and biopsy of the airway lesions is seldom, if ever, required [5]. Biopsy would reveal nodular areas consisting of ossified cartilaginous tissue in the subepithelial regions, with the underlying respiratory epithelium exhibiting a characteristic pattern and no atypia [6].
- Prakash, Udaya BS (2006) Uncommon Causes of Cough. CHEST, 129: 206S-219S.
- Tatar D, Senol G, Demir A, Polat G (2012) Tracheobronchopathia osteochondroplastica: four cases. Chin Med J (Engl) 125: 2942-2944.
- Nader K (2019) Tracheobronchopathia Osteochondroplastica. Mayo Clinic Proceedings 94(6): 49-950.
- Fois AG, Arcadu A, Santoru L, et al. (2016) Tracheobronchopathia Osteochondroplastica: a rare case report of a non-smoker and non-atopic patient, with a long history of wheezing since childhood. Multidisciplinary Respiratory Medicine 11: 16.
- Udaya BSP (2002) Tracheobronchopathia Osteochondroplastica. Semin Respir Crit Care Med 23(2): 167-176.
- Silveira MGM, Castellano MVCO, Fuzi CE, Coletta ENAM, Spinosa GN (2017) Tracheobronchopathia osteochondroplastica. J Bras Pneumol. 43(2): 151-153.
- Willms H, Wiechmann V, Sack U, et al. (2008) Tracheobronchopathia osteochondroplastica: A rare cause of chronic cough with haemoptysis. Cough 4(4).

Figures at a glance