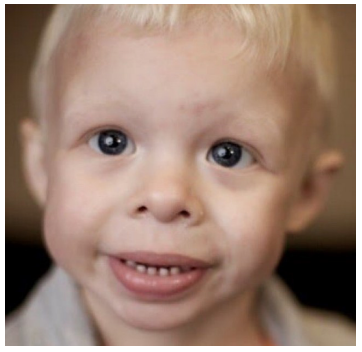
Figure 1: Characteristic facial features in Williams-Beuren syndrome (see text explanations). [13]
Patient |
I |
II |
III |
IV |
V |
|
Gender and age |
Female, 2 yrs. 2 |
Male, 5 yrs. 7 mos. |
Male, 7 mos. |
Female, 5 yrs. |
Male, 3 yrs. 3 mos. |
|
Pregnancy, term and mechanism of birth |
1st pregnancy; detached placenta V 1.m. 39 g.w. |
3rd pregnancy; no abnormalities 39+6 g.w. PVN |
1st pregnancy; 41 g.w. |
2nd pregnancy; 38 g.w., planned CS (maternal indications) |
2nd pregnancy; IUGR; 35 g.w., |
|
Neonatal period |
No pathological findings |
No pathological findings |
Neonatal depression, muscular hy- potonia, heart murmur with left-to- right shunt and pulmonary stenosis |
Neonatal depression; muscle hypotonia; atypical, mild pulmonary stenosis, systolic murmur, persistent foramen ovale |
Hemodynamically insignificant foramen ovale |
|
Anthropometric indicators at birth (WHO) |
Weight |
4th percentile, (-1.73 z-score) |
17th percentile, (-0.96 z- score) |
7th percentile, (-1.47 z-score) |
15th percentile, (-1.03z-score) |
<1st percentile, (-2.95 z-score) |
|
Height |
5th percentile, (-1.69 z-score) |
52nd percentile, (0.06 z- score) |
5th percentile, (-1.64 z-score) |
27th percentile, (-0.62 z-score) |
no data |
Head circumference |
37th percentile, (-0.32 z-score) |
no data |
17th percentile, (-0.95 z-score) |
37th percentile, (-0.32 z-score) |
no data |
|
BMI |
9th percentile, (-1.33 z-score) |
6th percentile, (-1.55 z- score) |
19th percentile, (-0.89 z-score) |
15th percentile, (-1.05 z-score) |
no data |
|
Current Anthro- pometric Indicators (WHO) |
Weight |
27th percentile, (-0.47 z-score) |
1st percentile, (-2.55 z- score) |
<1st percentile, (-2.18 z-score) |
9th percentile, (-1.34 z-score) |
3rd percentile, (-1.85 z-score) |
|
Height |
25th percentile, (-0.87 z-score) |
22nd percentile, (-0.76 z- score) |
<10th |
19th percentile, (-0.88 z-score) |
39th percentile, (-0.27 z-score) |
Head circumference (Hesse) |
33rd percentile, (-0.45 z-score) |
34th percentile, (-0.40 z- score) |
44th percentile, (-0.14 z-score) |
51st percentile, (-0.02 z-score) |
5th percentile, (-1.64 z-score) |
|
BMI |
44th percentile, (-0.17 z-score) |
<1st percentile, (-3.30 z- score) |
42nd percentile, |
16th percentile, (-0.98 z-score) |
<1st percentile, (-2.87 z-score) |
|
Anthropometric indicators according to the adapted nomograms for UiB |
Weight |
around the mean percentile of the normal weight-to- age chart |
below the mean but above the lower limit of the percentile range of the normal weight-to-age chart |
above the mean percentile of the normal weight-to-age chart |
within the lower half of the of the normal range on weight-to-age chart between the mean and -2SD |
within the lower half of the percentile range, between the mean of the weight-to- age chart and -2SD |
Height |
around the mean percentile of the normal height-to- age chart |
slightly above the mean percentile of the normal height-to-age chart |
around the mean percentile of the normal height-to-age chart |
around the mean percentile of the normal height-to- age chart |
above the mean percentile of the normal height-to- age chart (between themean and +2SD values) |
|
|
Head circum- ference (HC) |
above the mean percentile of the normal HC-to-age chart |
around the upper percentile range (+2SD) of the normal HC-to-age chart |
slightly above the upper percentile range (+2SD) of the normal HC- to-age chart |
within upper half of the percentile range (between the mean and +2SD values) |
within upper half of the percentile range (between the mean and +2SD values) |
Molecular genetic confirmation of the diagnosis |
At the age of 2 years Screening for microdeletions |
At the age of 4 years Screening for microdeletions |
at 3 months Targeted analysis |
at 4 months Targeted analysis |
At the age of 3 yearsTargeted analysis |
|
Phenotype |
Typical for infants with WBS facial phenotype; synophrys; Dentition - 1st tooth at the age of 6 mos. diastema, microdontia |
Typical for infants with WBS facial phenotype; bilateral epican- thus; Dentition - 1st tooth at 1 year + 7 months; diastema; microdontia |
Typical for infants with WBS facial phenotype with a well distinguished stellar iris pattern; bilateral epicanthusi Dentition - absent |
Typical for infants with WBS facial phenotype with a well distinguished stellar iris pattern; bilateral epicanthus; diastema, microdontia |
Typical for infants with WBS with sparse stellar pattern of the iris, bilateral epicanthus, diastema, microdontia |
|
Neurological and mental development |
Started walking — at 20 months; Fine motor skills - impairment; |
Started walking — at 4 yrs. Fine motor skills impaired; Speech - understands and answers questions, but has difficulty formulating whole words and phrases; Muscular hypotonia, highly vivid reflexes; |
Active back tummy rolling; actively crawls; tracks objects; grasps objects actively and steadily; makes baby sounds; Increased muscle tone of the limbs, brisk tendon reflexes up to clonus of the feet |
Started walking — at 2 yrs., after rehabilitation; Speech - first words at 2-yrs., very advanced, formulates sentences, communicates verbally, recites, sings, works with a speech therapist; Fine motor skills - difficult; Very advanced development in all areas for WBS; |
Started walking - at 16 mos. Fine motor skills - impaired; First words - at 2 yrs., intonation is age adjusted, well developed. |
|
Cardiovascular system |
CVS - no pathological findings; BP not measured |
CVS - no pathological findings; BP not measured |
Cvs - |
CVS - pulmonary stenosis improv- ing with age and SVAS; BP — not |
CVS - foramen ovale (closed); BP - not measured |
|
Gastrointestinal tract |
No complaints |
Feed difhculties - accepts only pureed foods, struggling with solids; Constipation |
Feeding difficulties - rejects lumpy foods, eats slowly; frequent regur- gitation. |
Feeding - requires more patience and time; the transition to some new foods takes longer. |
Feeding difhculties in transition to solid foods in infancy, has trouble with textures such as fruits and purees, eats very well on biscuit-lilce foods. Tendency to constipation |
|
Genitourinary system |
A normal find |
Cryptorchidism bilaterally; Ultrasound well differentiated pyra- mids, medullary nephrocalcinosis, unilateral hydronephrosis 1st degree |
No data |
Consistent follow- up; subtle bilateral nephrolithiasis |
Primary nocturnal enuresis; normal findings on Ultrasound |
|
Endocrine system; Calcium, Vitamin D, TSH |
Calcium and phosphate homeosta- sis - normal; TSH — increased, with normal values of FT3/FT4 — |
Hypercalcemia, hypercalciuria; Clinical hypothyroidism Hypovitaminosis D |
Calcium and phosphate homeostasis normal; TSH — normal. |
Calcium and phosphate homeosta- sis - normal; TSH — normal. |
Calcium and phosphate homeostasis - normal; TSH - no data. |
|
Connective tissue |
Joint hypermobility |
surgically repaired unilateral ingui- na1 hernia; Joint hypermobility |
Joint hypermobility |
surgically repaired bilateral ingui- nal hernias and |
surgically repaired umbilical hernia; Joint hypermobility |
|
Vision and hearing |
Hearing and vision not impaired, no medical data records available |
Hearing and vision not impaired, no medical data records available |
Hearing and vision not impaired, no medical data records available; hyperacusis |
Vision - initial signs of myopia; hearing - not impaired; hyperacusis |
Hearing and vision not impaired, no medical data records available; hyperacusis |
|
Behavioral features |
Loves music; Sleep difficulties; Hyperactivity |
Loves music, plays with other children with pleasure; Previously sleep difficulties, resolved by still ongoing therapy: falls asleep more easily and sleeps through the night; |
Sleep problems (difficulties in fall- ing asleep and sleeping through the night); Hyperactivity |
Loves music; No sleep problems; very communicative and friendly; Hyperactivity; attention deficit |
Loves music; Hyperactivity |
|
Time since counseling |
24months |
17 months |
16 months |
11 months |
9 months |
|
Outcomes añer genetic counseling |
Comprehensive parent education in WBS features and necessary followup schedule. Detailed plan for lifelong follow up for parents and pediatricians prepared.Individual growth charts for followup by the pediatrician prepared. Annual followup evaluation. Family further planning counseled. |
Comprehensive parent education in WBS features and necessary followup schedule. |
Comprehensive parent education in WBS features and necessary followup schedule. |
Comprehensive parent education in WBS features and necessary follow up schedule. Detailed plan for lifelong follow up for parents and pediatricians prepared.Individual growth-charts for follow up by the pediatrician prepared. Parents are exclusively compliant to the schedule and present annual reports of all check- ups to the genetic counselor. |
Comprehensive parent education in WBS features and necessary follow-up schedule.Detailed plan for lifelong follow-up for parents and pediatricians prepared.Individual growth-charts for follow-up by the pediatrician prepared.Family further planning counseled. |
|
Encountered complications |
Subclinical hypothyroidism and followup. |
Severe hypothyroidism identified - immediate supplementation. |
No |
No |
Severe dental problems and profound anxiety from doc- tors/dentists (anesthesia is discussed for treatment). |
|
Intervention results |
Physical therapy is very beneficial for development of motor skills. |
The family is skeptical about working with any specialist and prefers not to address the problem to teachers, despite the school offered special counseling. No further contact with our geneticist (living in another city). |
Very early intervention by physical therapy with incredible effect and very advanced motor skills development basic milestones |
Very early intervention by physical therapy with incredible effect and very advanced motor skills development basic milestones achieved within the normal (no- WBS) range. Very early intervention and working continuously with a speech therapist. |
Early intervention by physical therapy with very good effect; very good motor skills development. |
|
Table 1: Summarized phenotypes and clinical data for the five probands with genetically confirmed Williams syndrome. Abbreviations: yrs. - years; mos - months; g.w. - gestational week; CS - Cesarean section; 1.m. - lunar month; PVN - per vias naturalis (natural birth mechanism); IUGR - intrauterine growth retardation; WHO - world health organization; BMI - body mass index; HC - head circumference; CVS - cardio-- vascular system; BP - blood pressure; SVAS - supravalvular aortic stenosis; TSH - thyroid stimulating hormone.
Affected organ or body system: Symptoms for following-up |
Early childhood |
Child hood |
Adult hood |
Frequency |
RECOMMENDATIONS |
Thorough physical examination |
Yes |
Yes |
Yes |
NA |
At each physician visit or at least once annually. Ensure that the growth delay is not drastic, take measures as necessary |
CAUTION by SEDATION or ANESTHESIA!!! |
Yes |
Yes |
Yes |
||
ViSÎOI1: |
|
|
|
|
Ophthalmological examination lifelong once annually for any vision problems and for strabismus for all ages |
Strabismus (esotropia) |
Yes |
|
|
50 |
|
Hyperopia (hypermetropia) |
|
Yes |
Yes |
50 |
|
Cataract |
|
|
Yes |
|
|
Otorhinolaryngology: |
|
|
|
|
Otorhinolaryngology examination and audiogram, lifelong once annually. |
Recurrent otitis media; chronic otitis media |
Yes |
Yes |
|
50 |
|
Progressive sensorineural hearing loss |
|
Yes |
Yes |
65 |
|
Hypersensitivity to sounds |
Yes |
Yes |
Yes |
90 |
|
Dental status: |
|
|
|
|
Regular dental examinations and professional dental cleaning every 6 months up to 12 years of age; |
Enamel hypoplasia |
Yes |
Yes |
Yes |
95 |
|
Microdontia, Diastema |
Yes |
|
|
|
|
Malocclusion |
|
Yes |
Yes |
85 |
|
|
|
|
|
|
Basic examination at each physician |
|
visit for elevated blood pressure (of |
||||
|
3 or 4 extremities), heartfrequency, |
||||
|
heart tones. |
||||
|
Once annually, lifelong: |
||||
|
electrocardiogram (ECG). |
||||
|
At least once annually for age 1 to 5 |
||||
Cardiovascular problems: |
years and once in every 2 years |
||||
|
thorough examination by a |
||||
|
cardiologist with blood pressure |
||||
|
measurement on 3 or 4 |
||||
|
extremities,echocardiography, |
||||
|
Doppler sonography (for severe |
||||
|
stenosis incl. CT, MRI, |
||||
|
catheterization), ECG. |
||||
Basic examination |
Yes |
Yes |
Yes |
80 |
|
Supravalvular aortic |
Yes |
Yes |
Yes |
75 |
|
stenosis |
|
|
|
|
|
Supravalvular pulmoniC |
Yes |
Yes |
Yes |
25 |
|
stenosis |
|
|
|
|
|
Peripheral pulmonic |
Yes |
|
|
50 |
|
stenosis (PPS) |
|
|
|
|
|
Stenoses of other arteries |
|
Yes |
Yes |
20 |
|
Ventricular septal defect |
Yes |
|
|
10 |
|
(VSD) |
|
|
|
|
|
Arterial hypertension |
|
Yes |
Yes |
50 |
|
Prolonged QT interval |
|
Yes |
Yes |
13 |
|
|
|
|
|
|
Screening at diagnosis - single |
|
ultrasonographic (US) examination |
||||
|
(Doppler) of the kidneys and |
||||
|
renalarteries; US evaluation for |
||||
|
nephrocalcinosis; for bladder |
||||
|
malformations, diverticula. In adults |
||||
|
- USexamination once every 10 |
||||
Genitourinary problems: |
years. |
||||
|
Annually lifelong: serum BUN |
||||
|
(serum urea) and urinalysis; serum |
||||
|
creatinine - as necessary.In case of |
||||
|
complications (persistent |
||||
|
hypercalcemia, hypercalciuria, |
||||
|
nephrocalcinosis) - |
||||
|
consultationwith nephrologist. |
||||
Malformations |
Yes |
Yes |
Yes |
5 |
|
Enuresis (diurnal, |
|
|
|
|
|
nocturnal) |
|
Yes |
|
50 |
|
Nephrocalcinosis |
|
Yes |
Yes |
<5 |
|
Bladder diverticulosis |
|
Yes |
Yes |
50 |
|
Gastrointestinal problems: |
|
|
|
|
Continuous prevention of constipation. Each situation of abdominal pain should be addressed critically and having in mind that abdominal pain may be due to mesenteric artery stenosis(!) but alsoreflux, hiatal hernia, peptic ulcer, cholelithiasis, diverticulitis, ischemic bowel disease (due to motilityproblems, rectal prolapse, hemorrhoids, bowel perforation), and quite common - psychogenic (out offear). |
Feeding difficulties |
Yes |
Yes |
— |
70 |
|
Constipation |
Yes |
Yes |
Yes |
50 |
|
Diverticula of the colon |
|
Yes |
Yes |
30 |
|
Prolapse of the rectum |
Yes |
Yes |
— |
10 |
|
Skin and soft tissues: |
|
|
|
|
At least once annually, lifelong: surgical examination for hernias; |
Soft and hyperelastic skin |
Yes |
Yes |
Yes |
90 |
|
Inguinal hernia |
Yes |
|
|
40 |
|
Umbilical hernia |
Yes |
|
|
50 |
|
Premature greying of hair |
|
|
Yes |
90 |
|
Musculoskeletal problems: |
|
|
|
|
At least once annually, lifelong: orthopedic examination for joint hypermobility, contractures, scoliosis, kyphosis, lordosis. |
Joint hypermobility |
Yes |
Yes |
|
90 |
|
Joint contractures |
Yes |
Yes |
Yes |
50 |
|
Radio-Ulnar Synostosis |
Yes |
Yes |
Yes |
20 |
|
Kyphosis |
|
|
Yes |
20 |
|
Scoliosis |
|
Yes |
Yes |
18 |
|
Lordosis |
|
Yes |
Yes |
40 |
|
Pathological gait |
|
Yes |
Yes |
60 |
|
Calcium homeostasis and vitamin D: |
|
|
|
|
Serum calcium levels: once every 4 months up to 2 years of age, once every 2 years thereafter (urinelevels only if necessary). Consultation on nutrition and dietary calcium intake; dietary calcium corrections are made only under physician supervision and never by parents alone! |
Hypercalcemia |
Yes |
|
Yes |
15—45 |
|
Hypercalciuria |
Yes |
Yes |
Yes |
30 |
|
Vitamin D hypervitaminosis |
|||||
Endocrine problems: |
|
|
|
|
Strict follow—up of TSH levels (+FT3, FT4) once annually up to 3 years of age; thereafter once in 12to 24 months lifelong (no TAT and MAT measurement necessary - the hypothyroidism is caused bygland hypo-/aplasia). |
Hypothyroidism |
Yes |
Yes |
Yes |
5—10 |
|
Early (but not precocious) puberty |
|
Yes |
Yes |
20 |
|
Diabetes mellitus |
|
|
Yes |
15 |
|
Obesity |
|
Yes |
Yes |
30 |
|
Neurological problems: |
|
|
|
|
Thorough neurological examination once annually for signs of muscle hypotension, hypertension,cerebe1lar symptoms. Head MRI if Chiari is suspected. |
Hyperactive tendon reflexes |
|
Yes |
Yes |
75 |
|
Chiari type I malformation (caudal retraction of the cerebellar tonsils through the foramen magnum) |
Yes |
Yes |
Yes |
10 |
|
Central muscular hypotension |
|
Yes |
- |
80 |
|
Peripheral muscular hypertension |
Yes |
Yes |
Yes |
50 |
|
Cognitive and developmental problems: |
|
|
|
|
Physical monitoring according to the age-adapted WBS nomograms for height, weight and head circumference at each visit by physician up to 5 years of age and once annually thereafter until adolescence. |
Motor and physical developmental delay |
Yes |
Yes |
- |
95 |
|
Intellectual impairment (normal intelligence in up to 5%) |
|
Yes |
Yes |
75 |
|
Visuospatial cognitive impairment |
|
Yes |
Yes |
95 |
|
Behavioral features: |
|
|
|
|
Evaluation by psychologist/psychiatrist, symptomatic therapy if necessary (fear, depression, hyperactivity). Training in social skills. |
Attention Deficit Hyperactivity Disorder (ADHD) |
|
Yes |
|
65 |
|
Anxiety disorder (specific phobias, generalized anxiety) |
|
Yes |
Yes |
70 |
|
Sleep disorders |
|
Yes |
Yes |
65 |
|
Table 2: Summary of WBS clinical features and recommendations for follow-up of patients with Williams-Beuren syr+drome at different ages, as recommended by the American Academy of Pediatrics [2,7,16].
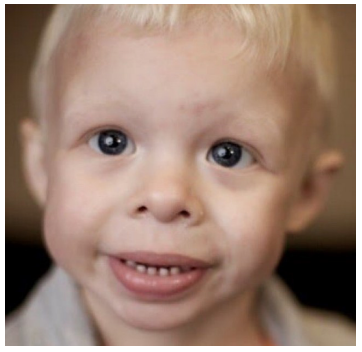
Figure 1: Characteristic facial features in Williams-Beuren syndrome (see text explanations). [13]
Tables at a glance
Figures at a glance