Difficult to Diagnose Chest Wall Neurofibroma: An Analysis of a Case Misdiagnosed for Ten Years
Received Date: April 15, 2024 Accepted Date: May 15, 2024 Published Date: May 18, 2024
doi: 10.17303/croa.2024.9.104
Citation: Chen Jianliang, Fu Jun, Si Wen, Liu Lianchun, Li Ruixiang, et al. (2024) Difficult to Diagnose Chest Wall Neurofibroma: An Analysis of a Case Misdiagnosed for Ten Years. Case Reports: Open Access 9: 1-13
Abstract
Neurofibroma of the chest wall, a benign tumor originating from intercostal nerve fibrocells, often presents with diverse clinical manifestations, leading to frequent misdiagnosis. This paper presents a case study of a 61-year-old woman who experienced right low back pain for ten years, initially misdiagnosed as intervertebral disc prolapse and spinal stenosis. After detailed clinical analysis, a chest wall neurofibroma was accurately diagnosed and surgically removed. Post-surgery, the patient's symptoms were completely resolved, and she resumed normal life. This case underscores the importance of thorough clinical analysis, accurate imaging, and the role of neurosurgeons in the complete resection of such tumors to ensure early recovery and reduce recurrence risks.
Keywords: Chest Wall Neurofibroma; Misdiagnosis; Intercostal Nerve Fibrocells; Clinical Manifestations; Microsurgery; Complete Resection; Neurosurgery
Introduction
Neurofibroma of the chest wall is a benign tumor originating from intercostal nerve fibrocells, with diverse clinical manifestations and often misdiagnosed [1]. This paper introduces a case of neurofibroma of the chest wall misdiagnosed for ten years. After detailed clinical analysis and clear diagnosis, the tumor was completely removed by microsurgery; the patient completely resumed the normal life and work. The author summarized the diagnosis and treatment process and recalled the experience of medical care.
Case Reporting
The patient was a 61-year-old woman with right low back pain for ten years. Ten years ago, the patient had low back pain and was unable to stand often. Sometimes radiating to the right abdomen. Several CT and MRI examinations in many large general hospitals were conducted, intervertebral disc prolapse and spinal stenosis was diagnosed. Related treatment were taken in many hospitals with traditional Chinese and western medicine, but the effect was not good. Recently, the patient's pain worsened, especially during coughing and deep breathing, sometimes he could not walk, and her back could not be straightened. She came to the hospital in March 2024.
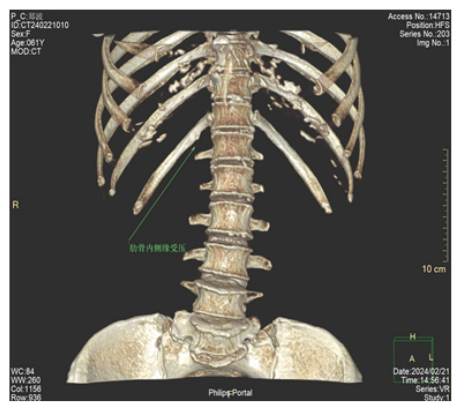
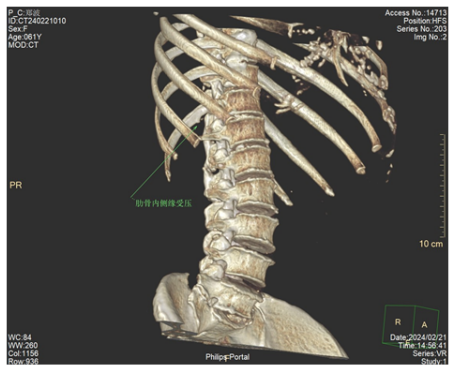
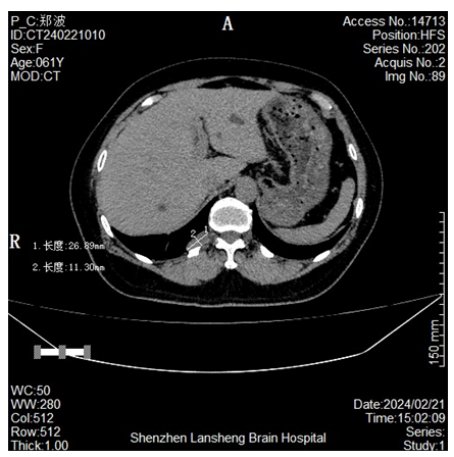
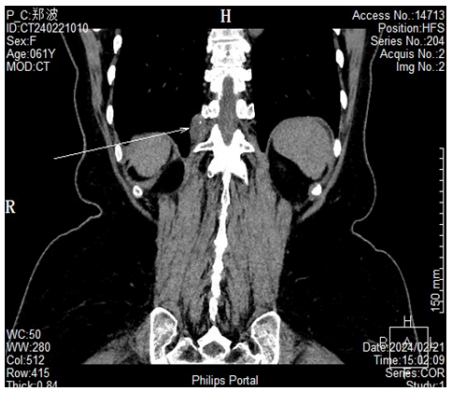
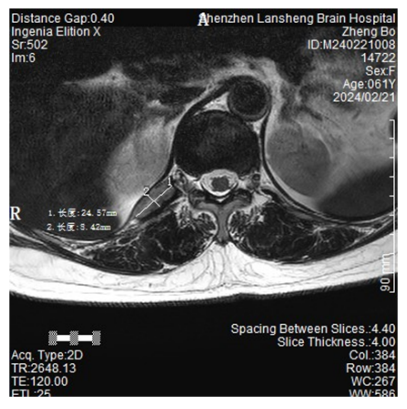
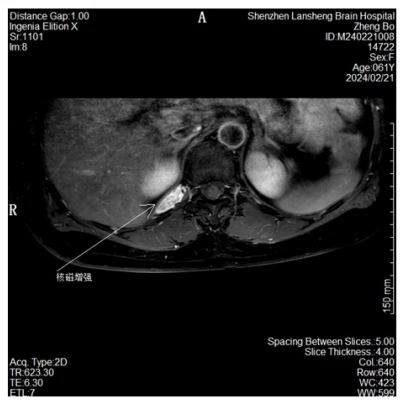
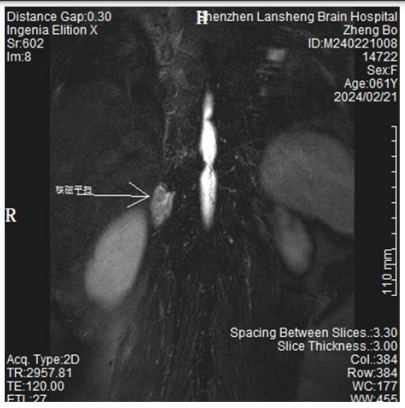
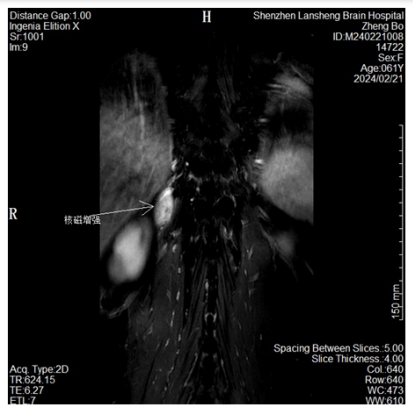
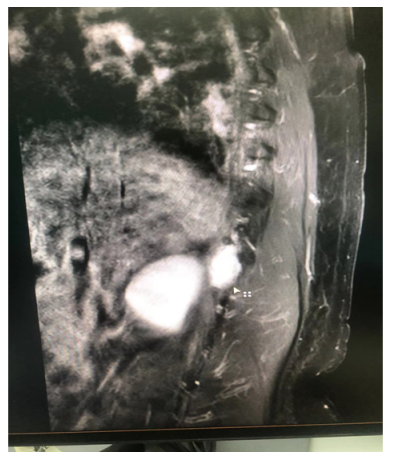
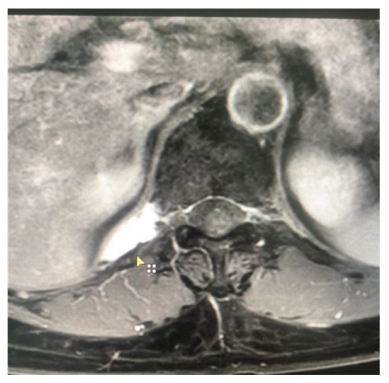
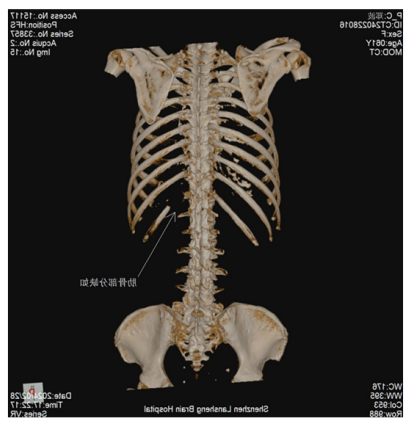
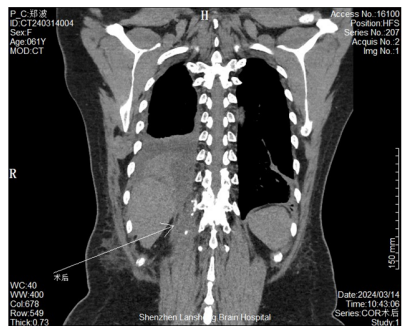
After careful inquiry of the medical history, the patient's pain was mainly waist band-like pain, which was aggravated during deep inhalation. In recent years, cannot straighten the back, the right shoulder backpack often slide down. On examination, the patient had a length of 161 CM from overhead to left plantar and 158 CM from overhead to right, suggesting the possibility of scoliosis, no nodules and brown pigment spots in the systemic skin. Physical examination found that the 3CM from the right side of thoracic spine 11 was tender. After percussion, the patient screamed pain, which lasted for about 20 seconds. Because she complained of unbearable severe pain, and the patient refused anymore percussion examination, which was too painful to bear. The author believes that such severe percussion pain is the manifestation of nerve root stimulation and neurofibroma could not be excluded. So the thoracolumbar CT examination was conducted. After repeated review by the radiology department doctors and the author, it was found that near the thoracic vertebrae 11 and 12, there was a lesion of about 4 cm 2 in size, attached to the T11 rib of the chest wall, and proximal adjacent to the transverse process of T11 vertebral body. It was proposed to be neurofibroma, and was admitted to the hospital for surgical treatment.
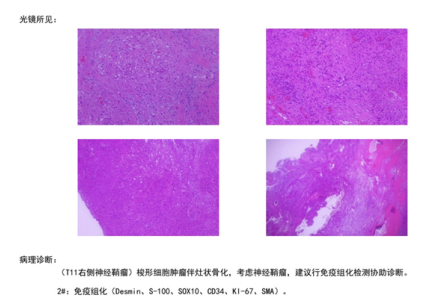
The paravertebral tumor resection was performed under general anesthesia. In the prone position, an 8CM long longitudinal incision was made 3CM aside the spinal column,, separated the muscle and the paraspinal space, without injured muscle fibers. After intraoperative C-arm X-ray repositioning to determine the lesion segment, 5CM of the T11 rib was removed with the bone bite forceps. After the resection a party of T11 ribs, ticked chest wall was found under microscopic exploration, tumor was suspected. We tried to dissect the tumor from pleural membrane to preserve the pleural membrane, but it was found that the tumor penetrated the chest wall and could not separate the tumor from the chest wall, and party of the tumor was covered by transverse processs, Finally, the transverse process and part of the lamina were removed under the microscope until the normal spinal membrane was clearly visible. The tumor was removed together with the pleura at the edge of the tumor, with the size of 4 * 4 * 3CM, pathological report: neurofibroma, confirmed by immunohistochemistry. Lung, diaphragm, and liver were seen after resection. No significant air leakage was observed in the operation field. The soft tissue was tightened to the pleural suture, drainage was placed, and the muscle was sutured to close the incision. After surgery, the patient's chest wall pain disappeared, percussion pain no longer existed, her back could normally straighten the spine, and the distance between the shoulders to the sole of the two sides was normal. There had been paroxysmal gastrointestinal distension and discomfort, after symptomatic treatment. Two weeks later, he was removed and discharged. Postoperative follow-up showed a good recovery with no signs of recurrence.
Literature Review and Discussion
Incidence
Chest wall neurofibroma is a manifestation of neurofibromatosis (Neurofibromatosis), and is usually associated with neurofibromatosis type 1 (NF 1). The incidence of neurofibromatosis is approximately 0.03%, and neurofibromatosis type 1 (NF 1) is the most common type. Based on the search results, the estimated incidence of NF 1 in China is 5 / 1 million. Neurofibroma of the chest wall is a relatively rare benign tumor, with a relatively low proportion in all chest tumors, and the specific incidence rate was not explicitly mentioned in the search results. Because of its diverse and unspecific clinical manifestations, it often leads to misdiagnosis and delay in treatment [2]. Most cases of chest wall neurofibroma reported in the literature show local masses and pain, and some patients may be accompanied by neurological dysfunction.
Clinical Manifestations
Clinical manifestations of NF 1 include cutaneous neurofibromas, and these tumors can be scattered or form plexiforms. Pleexiform neurofibromas may involve the main nerves and may develop malignant peripheral schwannoma (MPNST), in which survival may be extremely short. Neurofibroma of the chest wall may present as a local mass, may be asymptomatic or accompanied by pain, with a single local mass with radicular pain, mostly benign neurofibromas rather than NF 1.
Diagnosis
- Medical History Collection and Physical Examination: The patient's personal and family history should be known, especially if there is a history of genetic diseases, such as neurofibromatosis type 1 (NF 1). On physical examination, the skin should be checked for characteristic milk coffee spots, which is one of the diagnostic criteria for NF 1.
- CT Scan: can show the soft tissue density of the chest wall, may observe the tumor with clear, smooth or lobulated margin, adjacent rib erosion and calcification, in the early stage, only flat-like pleural thickening, which is difficult to diagnose in time.
- MRI: It is better than CT in understanding the relationship between tumor and peripheral tissue, which is helpful to evaluate the degree of tumor invasion and determine the nature of the tumor.
- PET / CT: The metabolic activity of tumors can be evaluated, helping to distinguish benign from malignant tumors, especially in distinguishing malignant peripheral schwannoma (MPNST) and benign neurofibroma in NF 1 patients.
- Pathological Tissue Biopsy: tissue samples were obtained by image-guided percutaneous puncture biopsy or surgical biopsy, and histological examination and immunohistochemical analysis were conducted to confirm neurofibroma and exclude malignant tumors.
- Genetic Testing: For patients with patients suspected of NF 1, genetic testing can be conducted to find out the presence of pathogenic variation in the NF 1 gene.
Treatment
Surgical resection is the preferred treatment for chest wall neurofibroma [12-15]. Reports in the literature show that complete resection of the tumor and part of the surrounding tissue can effectively reduce the recurrence rate. For tumors that cannot be completely removed, adjuvant radiotherapy may be considered. Literature reports, chest wall neurofibroma often diagnosed and treated by the thoracic surgeons, Intraoperatively, worry about the involvement of spinal cord and in order to avoid spinal cord injury, thoracic surgeons often failed to total resect the tumor underneath the transverse process or that inside the transverse process hole, leading to frequent recurrenceso the patient has to underwent multiple operations, to reduce recurrence, some thoracic surgeons invited neurosurgeon joint surgery, for some patients whether whose tumor has been totally removed , radiotherapy also be used after surgery. In this case, the operation was performed by neurosurgeon, total tumor resection has obtained under the microscope, tissue and organ damage can be reduced, the early fast recovery of the patient can be reached. However, because the follow-up time was short, whether and when the recurrence occurred still need a long follow-up.
Analysis of the Cause of Misdiagnosis
In this case, neurofibromas with segment of thorax 11 growing to the chest wall were not diagnosed for ten years, the following factors should be considered. First of all, the lesion is not typical, at early stage, tumor’s growth style was flat growth, tumor is not easy to be found, second, patients always complain if low back pain, inquiry in orthopedics, rehabilitation, geriatrics department without neurosurgeon’s and thoracic surgeon care, orthopedic doctor diagnosed of lumbar disc herniation, the followed doctor have preconceived conveniently thinking, patients and family members have accepted the diagnosis, Third, the lesion is not large, located in the thoracic paravertebral ribs and transverse process, imaging is difficult to find. The fourth factor is that clinicians were not well aware of the disease and not carefully examined the patient.
How to Reduce the Misdiagnosis Rate
Clinicians should integrate and analyse carefully the patient's clinical presentation, imaging characteristics, pathological findings and genetic information to establish a diagnosis. Imaging examination is the main diagnostic method [3-11]. Ultrasound, CT and magnetic resonance imaging have their own advantages in the diagnosis of chest wall neurofibroma [18]. Among them, magnetic resonance imaging has high value in the diagnosis of chest wall neurofibroma due to its high resolution and multiple sequence imaging ability. However, the diversity of growth patterns and clinical presentations often lead to misdiagnosis and delayed treatment. In this case, the diagnosis was not obtained for 10 years. After admission, the imaging doctor did not find the tumor after reading the film for the first time. The neurosurgeon found the patient with right lumbar-abdominal band-like pain, read the film with the radiologist again and the final clear diagnosis was made. Therefore, we should attach great importance to the medical history and clinical manifestations of patients, especially tenderness and percussion pain, and conduct comprehensive analysis combined with imaging examination, and should not ignore clinical routine examination due to modern advanced imaging examination. Doctors should read the film with the imaging department in person to improve the diagnostic accuracy and reduce misdiagnosis.
After discovering chest wall tumors, other types of chest wall tumors, such as chondroma, osteosarcoma, as well as metastatic tumors, should be excluded. For chest wall neurofibromas, especially when they are associated with NF 1, systemic MRI can be used to assess tumor burden, observe tumors not detected on physical examination and possible early detection of malignant transition. Importantly, MPNST should be highly suspected in patients with NF 1, which is an aggressive malignancy that requires prompt diagnosis and treatment, this case, without cutaneous pigmented spots, no multiple nodules, neurofibroma on pathological examination confirmed, the diagnosis. NF 1 can be ruled out.
Conclusion
Here we reported a case of chest wall neurofibroma misdiagnosis for ten years, through clinical analysis and careful imaging accurate diagnosis, with surgical microscope, resection of a part of the ribs and thoracic vertebra transverse process, the tumor was completely removed, the patient pain disappeared, two weeks after surgery the waist can stand straight, head distance to both feet returned to the same length. Under microscopy by a neurosurgeon, it facilitates complete tumor resection and reduces lung and adjacent tissue and organ damage, thus facilitating early recovery of the patient [17-19]. This case highlights the importance of clinical manifestations and clinical analysis in the diagnosis of disease, and reminds us that the awareness and diagnosis of chest wall neurofibroma should be improved in clinical work.
Acknowledgment
All the nurses of neurosurgery, the anesthesiology department of the hospital, all the medical staff of the operating room, the ultrasound imaging department, the hospital outpatient department, customer service and other logistics departments have given active cooperation and help in the diagnosis and treatment of patients. Thank you all here.
- Zhang Jinxiang, Huang Yongsheng, Li Kai, et al. (2021) Mechanism of Neurofibroma Pathogenesis: A Review. International Journal of Medicine and Health Guidance, 8.
- Li Beibei, Zou Xinxin, Fu Qingsong, et al. (2022) Misdiagnosis of Lumbar Disc Herniation as Intraspinal Neurofibroma: A Case Report. Anhui Medicine, 3.
- Yang Shuhui, Shang Liumeng, Zhong Yan, et al. (2023) CT and MRI Imaging Characteristics of Retroperitoneal Neurofibroma. Chinese Medical Equipment, 8.
- Han Lin, Xie Min (2022) Magnetic Resonance Imaging Features of Benign Retroperitoneal Paraganglioma and Neurofibroma. Imaging Research and Medical Application, 20.
- Zou Qiaoqiao, Wang Mingliang, Li Wenbin (2023) MRI Imaging Features of Atypical Intraspinal Neurofibroma. Biomedical Engineering and Clinical Medicine, 3.
- Han Pei, Tang Jie, Liao Hengbin, et al. (2023) Comparison of 18F-FDG PET/CT Findings between Benign and Malignant Peripheral Nerve Sheath Tumors. Medical Theory and Practice, 24.
- Li Dianwei, Liu Jinsong, Li Mei, et al. (2022) Clinical and Pathological Features of Intraspinal Neurofibroma. Neck and Back Pain Journal, 4.
- Gu Wuli, Zheng Manman, Liu Chuanxian, et al. (2022) Radiological Differential Diagnosis of Retroperitoneal Paraganglioma and Neurofibroma. Journal of Hepatobiliary and Pancreatic Surgery, 6.
- Sang Fei, Zhang Weiwei, Cheng Guanxun (2021) CT Diagnosis of Chest Wall Neurofibroma. Clinical Radiology Journal, 10.
- Yang Fan, Liu Jingyuan, Chen Yuan, et al. (2023) Clinical and Ultrasonographic Observations and Analysis of Neurofibromas at Different Anatomical Locations. Journal of Medical Imaging, 12.
- Liu Yichao (2022) A Case of Giant Primary Neurofibroma of the Lumbar Vertebrae. Practical Radiology, 6.
- Huang Wenpeng, Geng Shangwen, Li Liming, et al. (2022) A Case of Intraspinal Mixed Neurofibroma/Nerve Sheath Tumor. Chinese Journal of Interventional Imaging and Therapy, 2.
- Lin Guozhong, Ma Changcheng, Wang Zhenyu, et al. (2021) Minimally Invasive Microsurgical Treatment of C1-C2 Extramedullary Neurofibroma. Journal of Peking University (Medical Edition), 3.
- Lin Guozhong, Ma Changcheng, Wang Zhenyu, et al. (2020) Mid- to Long-Term Follow-up Results of Microsurgical Treatment of Intramedullary and Extramedullary Neurofibromas. Chinese Journal of Minimally Invasive Surgery, 5.
- Lin Guozhong, Ma Changcheng, Wang Zhenyu, et al. (2019) Microsurgical Minimally Invasive Treatment of Intramedullary Neurofibromas. Chinese Journal of Minimally Invasive Surgery, 4.
- Chen YY, Huang TW (2011) Intractable Chest Pain with Intercostal Nerve Schwannoma: Reply. Ann Thorac Surg. 111: 2084-5.
- Landriel F, Padilla Lichtenberg F, Ulloque-Caamaño L, Guerra E, Casto F, Hem S (2023) Carbon-Assisted Minimally Invasive Transtubular Approach for Intercostal Nerve Schwannoma..Oper Neurosurg (Hagerstown) 25: 449-52.
- Wu WT, Chang KV, Ozcakar L (2022) Ultrasound Examination Facilitated the Diagnosis of an Intercostal Schwannoma..Cureus. 14: e26079.
- Mason A Brown, JiaHao Hu, William Tisol, Paul Grebe, Matthew Howenstein (2022) Pre-operative embolization, surgical resection, and follow-up evaluation of a giant intercostal schwannoma Affiliations expand PMID: 35248891


Figures at a glance