Aggressive Vertebral Body Hemangiomas Causing Spinal Cord Compression During Pregnancy
Received Date: June 05, 2024 Accepted Date: July 05, 2024 Published Date: July 08, 2024
doi: 10.17303/croa.2024.9.105
Citation: Nina Capiro, MD, Noriko Salamon, MD, PhD, Sumit Dua, MD, MBA (2024) Aggressive Vertebral Body Hemangiomas Causing Spinal Cord Compression During Pregnancy. Case Reports: Open Access 9: 1-7
Abstract
Introduction: Vertebral hemangiomas are the most common benign tumors of the spine, often asymptomatic. During pregnancy, altered hemodynamics can rarely cause these hemangiomas to become symptomatic, leading to pain and neurological deficits. This case report discusses a pregnant woman with contiguous vertebral body hemangiomas causing compressive myelopathy.
Case Presentation: A 30-year-old woman at 31 weeks of gestation presented with progressive bilateral lower extremity numbness and weakness. MRI revealed aggressive vertebral body lesions at T3 and T4, resulting in severe spinal canal narrowing and cord compression. Initial management with Dexamethasone was followed by a multidisciplinary plan for cesarean delivery at 34 weeks, postponed due to acute neurological deterioration. The patient declined early delivery and underwent successful T3 laminectomy and epidural tumor resection with continuous fetal monitoring. Postoperative recovery was favorable, and she delivered a healthy baby at 37 weeks. Four months postpartum, she presented with recurrent symptoms and underwent embolization and corpectomy with spinal fusion, resulting in significant neurological improvement.
Discussion: This case illustrates the rare occurrence of symptomatic vertebral hemangiomas during pregnancy and emphasizes the need for a multidisciplinary approach. Imaging, especially MRI, is crucial for diagnosis, and treatment should be tailored based on the severity of symptoms and gestational age. Surgical intervention, though complex, can lead to positive outcomes when carefully planned.
Conclusion: Vertebral hemangiomas can pose significant challenges during pregnancy. A comprehensive, multidisciplinary approach is essential for effective management, balancing the health of both mother and fetus. This case contributes to the understanding of managing aggressive vertebral hemangiomas in pregnant patients, highlighting the importance of timely and coordinated care.
Keywords: Spinal Cord; MRI; Vertebral Hemangiomas; Pregnancy; Neurological Deficits
Introduction
Vertebral hemangiomas are the most common benign tumor of the spine, with a reported prevalence ranging from 11% to 26% in the general population [1]. Although vertebral hemangiomas are predominantly asymptomatic, the altered hemodynamics of pregnancy can rarely result in symptoms such as pain or neurological deficits. We present a case of a contiguous vertebral body hemangiomas causing compressive myelopathy during the third trimester of pregnancy.
Case
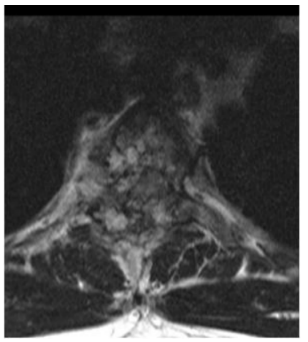
A 30-year-old, 31 weeks pregnant female with no significant past medical history was transferred from an outside hospital for two months of progressively worsening bilateral lower extremity numbness and weakness. On exam, the patient was found to have decreased sensation starting below her breasts, decreased motor strength in bilateral lower extremities, as well as bilateral Babinski reflex, clonus and hyperreflexia. MRI thoracic spine demonstrated aggressive T3 and T4 vertebral body lesions with extension into the epidural space and posterior elements at T3 with resultant severe spinal canal narrowing and cord compression (Figures 1, 2). These aggressive appearing lesions were correctly identified as vertebral body hemangiomas on imaging. Upon transfer from the outside facility, the patient was treated with Dexamethasone for spinal cord decompression. On hospital day 5, multidisciplinary meeting including neurosurgery, maternal fetal medicine, neuro intensive care unit, anesthesia and neonatal intensive care services concluded that plan would be for a controlled cesarean section at 34 weeks followed by one week of recovery before planned neurosurgery. However, following the multidisciplinary meeting, patient was noted to have acute worsening in neurological exam, with further decrease in strength of bilat eral lower extremities. Repeat MRI thoracic spine showed no significant change in degree of spinal canal stenosis or cord edema. Maternal fetal medicine recommended cesarean delivery prior to emergent neurosurgery, however the patient declined. Following discussion of procedural risks, patient underwent successful T3 laminectomy with resection of epidural vascular tumor, with continuous fetal monitoring during the procedure. Pathology findings were consistent with epithelioid hemangioma. Patient had progressive improvement in neurological exam following surgery. A dexamethasone taper was completed on post-operative day 6 and patient was transferred to inpatient rehab on post-operative day 7. Patient went on to have an uncomplicated cesarean delivery at 37 weeks.
However, approximately four months after delivery, the patient presented to the emergency department with two weeks of increased lower extremity spasticity and weakness. MRI of the thoracic spine demonstrated aggressive T3 and T4 hemangiomas with ventral epidural extension resulting in significant cord compression albeit not greatly changed from previous studies. The patient’s case was discussed at a multidisciplinary tumor board, where the consensus decision was for embolization of the lesions followed by surgical resection. One day after embolization of the right T4, left T4 and right T2 intercostal arteries with coils and polyvinyl alcohol performed by the neuro-interventional radiology team, the patient underwent corpectomy of T3 and T4 corpectomy with T1-T6 instrumented fusion with cage performed by the neurosurgery team. Despite preoperative embolization, there was an estimated blood loss of 2500cc during the procedure, requiring the transfusion of 3 units of blood intraoperatively. Patient was noted to have progressively improved bilateral lower extremity strength and sensation following the procedure. Prior to discharge, patient was noted to have 5/5 strength with only mildly diminished sensation in the bilateral lower extremities. At the patient’s first outpatient follow-up visit, she was noted have a normal sensory and motor exam with no new neurologic deficits.
Discussion
Epidemiology
Vertebral hemangiomas are often found incidentally on imaging studies, with less than 1% of these lesions resulting in symptoms [1]. When symptoms do occur, 55% of patients present with back pain alone while 45% present with neurological deficits [5]. Aggressive or compressive vertebral hemangiomas can result in symptoms secondary to extrinsic compression on the spinal cord due to bone expansion or extradural extension, spinal cord ischemia, vertebral body collapse or epidural hemorrhage [5,6].
Exacerbation in Pregnancy
As in the presented case, pre-existing vertebral hemangiomas can rarely become symptomatic during pregnancy, with less than 40 cases presented in the literature. As the gravid uterus exerts increasing extrinsic compression on the inferior vena cava and intra-abdominal pressures rise, blood flow to the vertebral venous plexus is increased, resulting in expansion and growth of previously asymptomatic vertebral hemangiomas [6]. Although hormonal changes have been implicated in the growth of vertebral hemangiomas during pregnancy, immune-histochemical studies have not been able to identify estrogen or progesterone receptors on vertebral hemangioma tissues [6]. Cases previously described in the literature most frequently present during the third trimester, with symptomatic vertebral hemangiomas most frequently occurring in the upper thoracic spine [3].
Imaging Characteristics
Radiographically, vertebral hemangiomas are classified as typical, atypical or aggressive [5]. On axial CT, typical vertebral hemangiomas are characterized by the “polka dot sign” with small punctate areas of high attenuation corresponding to sparse thickened trabeculae surrounded by hypodense stroma [5]. On sagittal and coronal CT, the vertically oriented thickened trabeculae produce the “corduroy sign” [5]. Typical vertebral hemangiomas are fat predominant lesions, resulting in T1 and T2 hyperintensity on MR imaging [7]. Typical lesions demonstrate variable enhancement on post-contrast images; however, the extradural components tend to enhance more than the intravertebral component [5,7].
On CT, atypical vertebral hemangiomas often have the typical “polka dot sign,” but may also have more nonspecific findings such are cortical expansion or lysis and extra-osseous soft tissue extension [5]. The distinction between typical and atypical vertebral hemangiomas is predominantly based on MRI appearance [5]. Atypical vertebral hemangiomas contain less fat and are more vascular than typical lesions [5]. As a result, atypical vertebral hemangiomas are T1 iso- or hypo-intense and very T2 hyperintense with variable enhancement on post-contrast images [5]. Atypical lesions with more vessels are more likely to be symptomatic [5].
Aggressive vertebral hemangiomas usually have atypical features, in addition to extension beyond the vertebral body, cortical destruction, and invasion of epidural and paravertebral spaces [5].
Workup for aggressive lesions may involve angiography to determine vascularity, identify feeding and draining vessels, and evaluate blood supply to the cord [5]. Angiography usually demonstrates dilation of vertebral body arterioles, multiple blood pools in the capillary phase and intense opacification extending throughout the entire vertebral body [5].
Diagnosis of atypical and aggressive VHs is difficult because they can mimic primary osseous malignancies or metastases [5]. As a result, CT and MRI are usually performed in order to narrow the differential diagnosis [5]. However, in pregnancy MRI is the first diagnostic choice, as it spares the patient and the fetus from exposure to ionizing radiation [7]. Additionally, MRI is best for visualization of degree of epidural extension and cord compression.
Treatment
Treatment options for symptomatic vertebral hemangiomas include conservative medical therapy, vertebroplasty, transarterial embolization, direct intralesional ethanol injection, radiotherapy, surgery, or a combination thereof [5]. However, no class I evidence exists regarding management [3]. As a result, treatment is based on patient symptoms and lesion imaging features [5]. Special considerations must be taken when patients present symptomatically during pregnancy. For example, radiotherapy is relatively contraindicated during pregnancy and transarterial embolization can be complicated by vascular injury and results in radiation exposure from fluoroscopy [6]. Furthermore, surgical intervention during the antepartum period presents an increased risk of preterm labor and increased risk of bleeding [3]. Laminectomy may be temporarily effective and used for emergency decompression, however symptoms often recur and more definitive treatment is typically necessary [6]. Despite increased surgical risk, review of nine cases in the literature with antepartum surgical intervention including laminectomy or vertebroplasty demonstrated favorable or good outcomes in all cases [3].
Chi et al present an algorithm for management of symptomatic vertebral hemangiomas in pregnant patient. Patients at 36 weeks gestation or greater should be treated conservatively with observation and pain control. If neurological function worsens, induction of labor with subsequent surgical intervention is suggested. Between 32- and 36-weeks’ gestation, surgery is reserved for cases of severe paraplegia. At less than 32 weeks gestation, antepartum surgery should be considered only for severely symptomatic patients [4,6]. Our patient underwent laminectomy at approximately 32 weeks gestation due to progression of neurologic deficits.
- Slon V, Stein D, Cohen H, Sella-Tunis T, May H, Hershkovitz I (2015) Vertebral hemangiomas: their demographical characteristics, location along the spine and position within the vertebral body. Eur Spine J. 24: 2189.
- Fereydonyan N, Taheri M, Kazemi F (2017) Recurrent symptomatic vertebral hemangioma during two consecutive pregnancies: Case report and review of the literature. Surg Neurol Int. 8: 105.
- Gupta M, Nayak R, Singh H, Khwaja G, Chowdhury D (2014) Pregnancy related symptomatic vertebral hemangioma. Ann Indian Acad Neurol. 17: 120-2.
- Chi J, Manley G, Chou D (2005) Pregnancy-related vertebral hemangioma. Case report, review of the literature, and management algorithm. Neurosurg Focus. 19: E7.
- Gaudino S, Martucci M, Colantonio R, Lozupone E, Visconti E (2015) A systematic approach to vertebral hemangioma. Skeletal Radiol. 44: 25.
- Slimani Q, Jayi S, Alaoui F, Bouguem H, Chaara H, Fikri G, et al. (2014) An aggressive vertebral hemangioma in pregnancy: a case report. J Med Case Rep. 8: 207.
- Kiroglu Y, Benek B, Yagci B, Cirak B, Tahta K (2009) Spinal cord compression caused by vertebral hemangioma being symptomatic during pregnancy. Surg Neurol. 71: 487-92.


Figures at a glance