Delayed Hydrothorax in a Severe Case of Wernicke Encephalopathy
Received Date: June 20, 2024 Accepted Date: July 20, 2024 Published Date: July 23, 2024
doi: 10.17303/croa.2024.9.201
Citation: Ahlers N, Stirbulescu C, Arnold M, Deeg S, Teipel M, Kermer P (2024) Delayed Hydrothorax in a Severe Case of Wernicke Encephalopathy. Case Reports: Open Access 9: 1-5
Abstract
Cannulation of a central vein is a very frequent procedure not only on neuro-intensive care units. Complications range from arterial punctures and pneumothorax during the insertion procedure to delayed complications. These include infection, thrombosis, fracture and embolization, catheter migration, venous erosion, and hydrothorax or hydromediastinum, with the latter being a very rare event. The patient presented with signs of Wernicke encephalopathy and was alimented with parenteral nutrition and supplemented with thiamine via a left-sided subclavian central vein catheter. She developed respiratory failure on day 8 post admission due to delayed bilateral hydrothorax. Following bilateral thoracic drainage and mechanical ventilation as part of intensive care the patient recovered and was released in neurological rehabilitation. This case of late hydrothorax should prompt physicians to re-evaluate the necessity of intensive care procedures on a daily basis especially when alimentation is carried out via the left subclavian vein.
Keywords: Wernicke Encephalopathy; Central Vein Catheter; Delayed Hydrothorax
Introduction
Wernicke encephalopathy (WE) is a severe and life-threatening condition resulting from insufficient supplementation with vitamin B1 (thiamine). The classical clinical triad of symptoms indicating WE is ocular signs, cerebellar dysfunction and confusion/delirium [1]. About 50% of cases are associated with alcohol abuse, while other causes comprise gastrointestinal procedures like bariatric surgery, genetic factors, hyperthyroidism, starvation, hyperemesis, infections and chemotherapy [2]. Suspected or manifest WE should lead to immediate vitamin B1 supplementation. It should be given, before any carbohydrate, 200 mg thrice daily, preferably intravenously [1]. If misdiagnosed or untreated, WE culminate in permanent brain damage and a mortality rate of 20% [3]. Other causes for delirium might distract from WE diagnosis which range from drug intoxication (e.g. lithium, opioids), poisoning, metabolic abnormalities to infectious or inflammatory brain disorders [4]. Severe WE cases are usually managed by a multidisciplinary team on intensive care units where parenteral treatment, if necessary, usually is executed through central venous catheters. As a matter of principle, such cannulation procedures are associated with complications ranging from arterial punctures and pneumothorax during the insertion procedure to delayed complications including infection, thrombosis, fracture and embolization, catheter migration, venous erosion, and hydrothorax. These have to be closely monitored especially in cases in which long-term parenteral nutrition is often inevitable like in the case of WE presented here.
Case Presentation
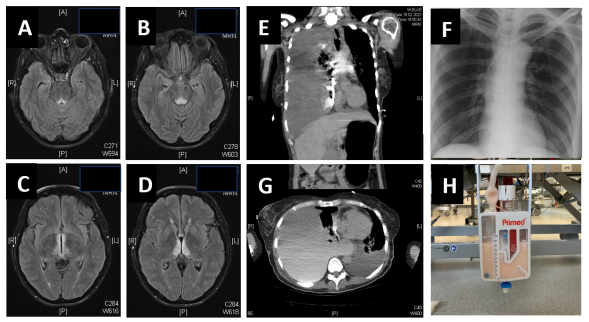
A 54 year-old female was admitted to our intensive care unit due to soporific state of consciousness after being found by rescue services lying in bed unresponsively. Third-party anamnesis revealed that she had been without food and fluids for several days. Medical history indicated potential alcohol and substance abuse. Oral medication included lithium, aripiprazole and lorazepam based on the diagnosis of a bipolar disorder. However, she did neither benefit from naloxone nor flumazenil application. Instant laboratory exams showed substantially increased liver enzymes and ruled out intoxication as well as meningoencephalitis. The patient was referred to our interdisciplinary ICU where neurological examination showed an alert person only partly able to make eye-contact due to divergent bulbi and insufficient motoric reaction upon stimulation. MRI scans revealed classic signs of WE (Figure 1A-D) and intravenous thiamine substitution as well as high-caloric nutrition was initiated immediately via right-sided jugular central venous catheter which was switched to left subclavian the following day due to dislocation. Correct placement was proven by thoracic X-ray exam (Figure 1F). Nutrition through naso-- gastral tube failed repeatedly due to incompliance resulting in continuous central venous administration. On hospital day 8 she experienced a sudden impairment of respiration with tachypnoea and reduced oxygen saturation resulting in analgo-sedation and mechanical ventilation. Thorax-CT scans showed bilateral pleural effusion with massive accentuation on the right side, mild pericardial effusion and mediastinal shift (Figure 1E, G). Bilateral pleural drainage revealed infuso-/hydrothorax with parenteral nutrition solution mixed with blood (Figure 1H) from the correctly positioned subclavian catheter indicating vessel perforation. Central line was switched to femoral vein, no subsequent pneumothorax, hematothorax or other complications occurred. The patient slowly recovered partly also regarding her neurological deficits. However, course was complicated by transient hypoactive delirium. Antipsychotic medication was changed to aripiprazole and olanzapine. She could be released in substantially improved condition for early neurological rehab on day 45 post-admission.
Discussion
Delayed infuso-/hydrothorax through central venous catheterization is a very rare but, if not detected instantly, often fatal event. Using the terms delayed hydrothorax revealed 79 PubMed hits since 1977 of which only 22 were in English and associated with placement of a central line mostly via the left subclavian vein. While most reports describe single case reports [e.g. 5-11], a small case series published in 1984 [12] indicated increased risk for delayed hydrothorax when central catheters are inserted from the left side. Similarly, Duntley et al. 1992 [13] summarized 8 cases, 7 of which had a left-sided catheter placement. 6 of these 7 left-sided catheters abutted the superior vena cava wall within approximately 45 degrees of perpendicular again suggesting left-sided catheter placement as important risk factor for vascular erosion. This risk might be further increased by hyperalimentation with nutritional fluids due to osmotic injury to the wall of the vein [14]. Besides thorough examination of adequate flow through central catheters, we therefore recommend to use soft, pliable catheters sutured firmly in place to avoid this delayed complication. Right-sided line placement is preferable to left-sided placement because of the anatomic relationships.
Conclusion
Our case of late infuso-/hydrothorax should prompt physicians to re-evaluate intensive care procedures on a daily basis leading to termination, if applicable. Central line insertion from the right side should be preferred to avoid this often-fatal complication, especially when used for hyperalimentation.
Consent for Publication
Patient gave written consent for publication of hercase
Data Availability
The clinical and laboratory data used to support the findings of this study are available from the corresponding author upon request.
Conflicts of Interests
Authors declare no competing interests
- Galvin R, Bråthen G, Ivashynka A, Hillbom M, Tanasescu R, Leone MA, et al. (2010) EFNS guidelines for diagnosis, therapy and prevention of Wernicke encephalopathy. Eur J Neurol, 17: 1408‑18.
- Ota Y, Capizzano AA, Moritani T, Naganawa S, Kurokawa R, Srinivasan A (2020) Comprehensive review of Wernicke encephalopathy: pathophysiology, clinical symptoms and imaging findings. Jpn J Radiol, 38: 809-20.
- Chandrakumar A, Bhardwaj A, 't Jong GW (2018) Review of thiamine deficiency disorders: Wernicke encephalopathy and Korsakoff psychosis. J Basic Clin Physiol Pharmacol, 30: 153-62.
- Habas E, Farfar K, Errayes N, Rayani A, Elzouki AN (2023) Wernicke Encephalopathy: An Updated Narrative Review. Saudi J Med Med Sci, 11: 193-200.
- Wright JE (1982) Hydrothorax: a delayed complication of parenteral nutrition via a central venous catheter. Aust Paediatr J, 18: 216-8.
- Iberti TJ, Katz LB, Reiner MA, Brownie T, Kwun KB (1983) Hydrothorax as a late complication of central venous indwelling catheters. Surgery, 94: 842-6.
- Colón R, Frazier OH (1985) Right hydrothorax after left subclavian and internal jugular vein catheterization: a delayed complication. Tex Heart Inst J, 12: 389-92.
- Thomas CJ, Butler CS (1999) Delayed pneumothorax and hydrothorax with central venous catheter migration. Anaesthesia, 54: 987-90.
- Kunizawa A, Fujioka M, Mink S, Keller E (2010) Central venous catheter-induced delayed hydrothorax via progressive erosion of central venous wall. Minerva Anestesiol, 76: 868-71.
- Aggarwal R, Soni KD (2015) Delayed massive hydrothorax following subclavian catheter insertion: an unusual complication. Crit Care Nurs Q, 38: 405-8.
- Chica J, Ballén NP, Aguillon KJ, Rugeles SJ (2021) Hydromediastinum and hydrothorax as delayed complications of peripherally inserted central catheter used for total parenteral nutrition: A case report. Int J Surg Case Rep, 86: 106247.
- Molinari PS, Belani KG, Buckley JJ (1984) Delayed hydrothorax following percutaneous central venous cannulation. Acta Anaesthesiol Scand, 28: 493-6.
- Duntley P, Siever J, Korwes ML, Harpel K, Heffner JE (1992) Vascular erosion by central venous catheters. Clinical features and outcome. Chest, 101: 1633-8.
- McDonnell PJ, Qualman SJ, Hutchins GM (1984) Bilateral hydrothorax as a life-threatening complication of central venous hyperalimentation. Surg Gynecol Obstet, 158ss: 577-9.

Figures at a glance