The Expression of CD44, CD133 and NLR in Patients with Non-Small Cell Lung Cancer and their Clinical Significance for Prognosis Evaluation
Received Date: January 27, 2023 Accepted Date: February 25, 2023 Published Date: February 28, 2023
doi: 10.17303/jcrto.2023.11.101
Citation: Xinfu Liu, Lijie Sima, Huajie Yin, Tengda Zeng (2023) The Expression of CD44, CD133 and NLR in Patients with Non-Small Cell Lung Cancer and their Clinical Significance for Prognosis Evaluation. . J Cancer Res Therap Oncol 11: 1-12
Abstract
Objective: To explore the relationship between CD44, CD133 and neutrophil-to-lymphocyte ratio (NLR) and the pathological characteristics of non-small cell lung cancer (NSCLC) and their significance in prognostic evaluation.
Methods: A total of 120 patients with stage I to IV NSCLC and 40 normal tissues with a distance of more than 5 cm from the cancerous tissue were randomly selected as clinical research samples. The NLR of the experimental group and the control group were compared, and the relationship between CD44, CD133, NLR and the pathological characteristics and prognosis of NSCLC patients was analyzed.
Results: The positive expression rates of CD44 and CD133 in NSCLC cancer tissues were significantly higher than those in adjacent tissues (P<0.05); the serum NLR in the experimental group was significantly higher than that in the control group (P<0.05). CD44 and CD133 protein positivity was not related to the gender, age, tumor location, tumor diameter and clinical stage of NSCLC patients (P>0.05), but was related to the degree of tissue differentiation and lymph node metastasis (P<0.05), while the tumor diameter was >3 cm The NLR of NSCLC patients with lymph node metastasis was significantly higher than that of other similar items (P<0.05), and the study results also showed that the 2-year survival rate of the NLR low group was 89.86%, which was significantly higher than that of the NLR high group (32.26% (χ2). =35.198, P<0.05); but the 2-year survival rate of the CD44-negative group (85.71%) was not significantly different from that of the CD44-positive group (69.77%) (P>0.05).
Conclusion: CD44, CD133, and NLR are closely related to the pathological characteristics of NSCLC patients. Theexpression levels of CD133 and NLR affect the prognosis and survival rate of NSCLC patients, and can be used as effective markers for the biological behavior and prognosis evaluation of NSCLC patients.
Keywords: Non-Small Cell Lung Cancer; Stem Cell Markers; CD133; CD44; Neutrophil-To-Lymphocyte Ratio; Prognosis
Introduction
Lung cancer is the leading cause of cancer-related death in men and women worldwide, with an estimated 2.09 million new cases of lung cancer and 1.76 million deaths in the globocan201database [1]. Lung cancer can be divided into two main categories according to the pathological type: non-small cell lung cancer (NSCLC) and small cell carcinoma, and NSCLC is the most common type of lung cancer, accounting for 80-85% of all lung cancer cases [2,3]. Despite the discovery and application of new standard treatments, the majority of NSCLC patients, who have lost the opportunity of radical surgery at the time of diagnosis, belong to locally advanced or advanced lung cancer due to the lack of effective screening instruments in the early stages of lung cancer. Thus the current 5-year relative survival rate of lung cancer is still 18% [4-6], and the poor outcome of lung cancer can be attributed to the high incidence of metastasis at diagnosis and high rec- urrence frequency after radical resection [7,8].
Stem cells regenerate all tissues and evoke self-renewal in order to generate an adequate cell supply for tissue repair. Moreover, emerging evidence supports the cancer stem cell hypothesis that malignancies are initiated and maintained by progenitor cells within tumors that share similar biological characteristics with normal adult stem cells [9-11]. Several biomarkers have been used in stem cell research to identify the characteristics of lung cancer stem cells. Among them, CD44 and CD133 are the two most commonly used stem cell markers [12]. Meanwhile, studies have found that cancer stem cells and tumor recurrence and metastasis are closely related, and the expression amounts of cancer stem cell markers CD44 and CD133 are correlated with the efficacy of chemotherapy and prognosis in a variety of tumors [13, 14]. Neutrophils are key first responders to infection sites and tissue damage and play an important role in host defense. Neutrophils are also confined to the tumor microenvironment (TME) in a variety of human cancers, and neutrophil infiltration and an increased neutrophil to lymphocyte ratio in tumors are often associated with poor patient outcomes [15-17]. Thus, there is growing interest in understanding the role of neutrophils in the developing tumor microenvironment and how their presence alters adaptive immune responses. With recent advances in T cell-mediated immunotherapy, a better understanding of the role of innate leukocytes in tumors and tumor initiating niches, as well as the signals that mediate their recruitment to improve the efficacy of immunotherapy and patient outcome, is required, and therefore, it is of great value to analyze the relationship of CD44, CD133, and NLR with pathologic features of NSCLC and their clinical significance in prognosis.
Clinical Data and Methods
General Information
The pathological samples of 120 NSCLC patients who were pathologically confirmed by surgical resection or needle biopsy in our hospital between January 2020 and December 2021 were selected as study subjects. Cancerous tissue samples were a total of 120 cases in the observation group, in which 40 cases of normal tissues that were more than 5 cm away from cancerous tissues were randomly selected as the control group, all specimens were used paraffin embedding. The 120 patients included 69 males and 51 females; Age range 45-75 years, mean (53.25 ± 6.02) years; According to the TNM stage, 8 subjects were in stage I, 34 subjects in stage II, 40 subjects in stage III and 38 subjects in stage IV, and all subjects underwent complete case analysis, and this study was performed with the approval of the ethics committee of the hospital.
Inclusion criteria: cytologically or histologically confirmed non-small cell lung cancer; There are well-established imaging modalities including B-ultrasound, CT, and MRI to assess lung cancer stage according to the eighth edition of the TNM staging of lung cancer; Without any treatment, including radiotherapy, chemotherapy, targeted therapy, immunotherapy and traditional Chinese medicine and other anti-tumor treatment; First line regimens are all platinum containing doublet chemotherapy consisting of pemetrexed, paclitaxel, albumin paclitaxel, gemcitabine, and docetaxel; Treatment efficacy was assessed radio- graphically at both 2 and 4 cycles after chemotherapy; There are well-established reports of blood routine tests in the Department of laboratory medicine of Shaoyang central hospital to calculate NLR, and the report of blood routine needs to be within 1 week before chemotherapy
Exclusion criteria: had used hormone or hematopoietic factor therapy within nearly 1 month; Pathologically confirmed small cell lung cancer or combined with other malignancies; 3. Combined acute and chronic infectious disease as well as combined degree I above myelosuppression; Combined with severe heart, liver, kidney and other important organ dysfunction, combined with blood system diseases; Staging could not be assessed before treatment and efficacy could not be evaluated after treatment.
Study Methods
Detection of CD44 and CD133 Antigens by Immunohistochemical Staining [18]
Paraffin specimens collected in the pathology department were deparaffinized on xylene, deparaffinized and eluted with graded ethanol, and then incubated in 3% hydrogen peroxide solution for 20 min to inactivate endogenous peroxidases. The sections were immersed in citrate buffer (0.01 mol / L, pH 6.0) and kept in a microwave oven for antigen retrieval for 15 min. After another wash with phosphate buffered saline (PBS), 5% BSA blocking solution was added dropwise, and incubation for 20 min at room temperature, primary antibodies were added in grouped drops, anti-CD44 mAb dilution was 1:100, anti-cd133 mAb was diluted 1:150, and placed on ice overnight at 4 ° C. The sections were washed three more times in PBS, secondary antibody was added dropwise, reagent SABC was added dropwise, DAB was modestly stained, hematoxylin counterstained, dehydrated, and DPX was mounted. The staining intensity was judged by semiquantitative integration, and an average of 5 high-power fields randomly observed for each sample was assigned a score of 0 for ≤ 5%, a score of 1 for > 5% - 25%, 2 for > 25% - 50%, 3 for > 50% - 75%, and 4 for > 75%. The positive cells expressed the following staining depths: no staining, light yellow, brownish yellow and tan, corresponding to 0, 1, 2 and 3 points, respectively, the score of multiplying the two points of staining intensity and pigmentation depth from 0 to 2 points was assigned as negative, 3 to 4 points as weak positive, 5 to 8 points as moderate positive, 9 to 12 points as strong positive, and ≥ 3 points were drawn up in this study as positive expression of CD44 or CD133. A known positive patch was used as a control, and PBS solution instead of the primary antibody was used as a negative control.
NLR Assay [19]
For 120 NSCLC patients, we collected preoperative elbow vein blood from NSCLC patients and extracted the complete blood count test results of lymphocytes, monocytes, neutrophils, eosinophils, baso- phils, leukocytes, erythrocytes, and platelets. Baseline values were calculated closest to the date of treatment or within 60 days before the date of treatment, with up to 97% of patients having the value within 2 weeks before treatment initiation. Laboratory values occurring within a time frame (e.g. 2-8 weeks) were calculated as the average of all laboratory values recorded for the individual within that time frame and finally the NLR was derived following the above data processing.
Prognostic Analysis
With regular visits to the hospital or telephone follow-up, the survival time was defined as the starting point using the date of patient's diagnosis, and the follow-up ended on the date (2 years) or patient's death time as the end point.
Analytical Indexes
1.The expression of CD44, CD133, and NLR in each group was compared between NSCLC tissues and normal tissues;
2.The relationship between the expression of CD44, CD133 and NLR in tumor tissues and clinicopathological characteristics;
3.The association between the exp- ression of CD44, CD133, and NLR and the prognosis of NSCLC patients was obtained by telephone follow-up statistics for 2-year survival of patients
Statistical Methods
Spss20.0 statistical software was used to analyze the related data, and the counting data were expressed as cases and percentages, with a χ2-Test between groups. The measurement data are presented as (x±s), and the Kaplan Meier method was used to calculate patient survival, and the Mann Whitney U test was used for comparison between groups with ordered categorical data. The cut-off value of peripheral blood NLR for predicting patient efficacy was determined by receiver operating characteristic curve (ROC), and the test level was considered statistically significant at P < 0.05.
Results
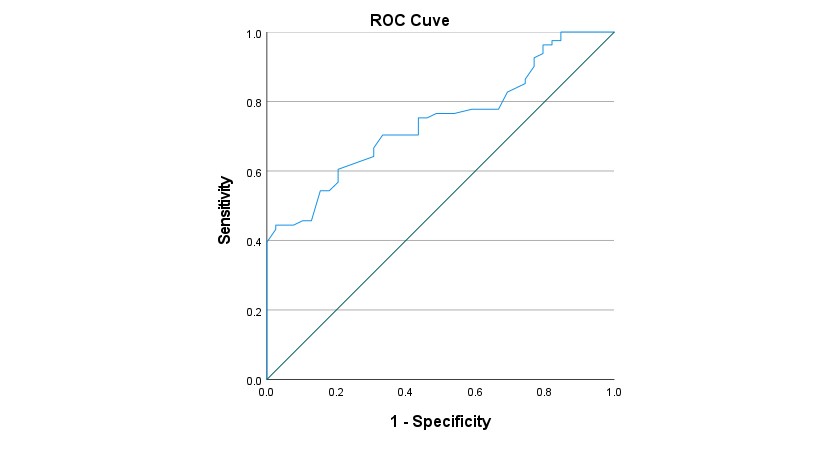
ROC Curve and Limits of NLR
The results of ROC curve analysis for NLR prediction of patient efficacy are shown in Figure 1. ROC curves were drawn with patient treatment efficacy as the status variable and NLR as the test variable. The results showed that the area under the curve of NLR was 0.742 (0.656-0.829), corresponding to a p value of 0.000, which indicated that NLR was statistically significant in predicting patient outcomes. The optimal cutoff point for NLR was 2.645, corresponding to a sensitivity of 60.5%, a specificity of 79.5%, and a Youden index of 0.400. According to the cut-off point, 8 patients were classified into the NLR high expression group (≥ 2.645), which accounted for 48.3%, and 62 patients were classified into the NLR low expression group (< 2.645).
The Relationship between CD44, CD133, and NLR and the Pathological Characteristics of NSCLC Patients
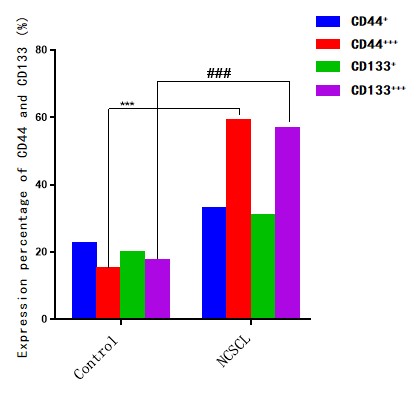
A total of 120 lung cancer patients with stages I to IV were included in this study, and their tumor samples were examined by immunohistochemistry for the expression of CD44, CD133, and the expression of each group was defined as high and low according to the following figure (Figure2); From the following table (table1), we found that CD44 and CD133 protein positivity was not associated with patients' gender, age, tumor location, tumor diameter, pathological type and clinical stage (P > 0.05), and was associated with the degree of tissue differentiation as well as whether lymph nodes were metastatic or not (P < 0.05); However, after statistical analysis, we found that both stem cell markers were significantly highly expressed in NSCLC patients (shown in Fig.3), 59.20% (71 patients) had high expression of CD44, 56.67% (68 patients) had high expression of CD133; Meanwhile, the results of table1 showed that the NLR of NSCLC patients with lymph node metastasis was significantly higher when the tumor size was ≥ 3 cm in diameter and the clinical stage (P < 0.05) than that of the other groups.
Analysis of the Relationship between the Expression of CD44, CD133 and NLR and the Prognosis of NSCLC Patients
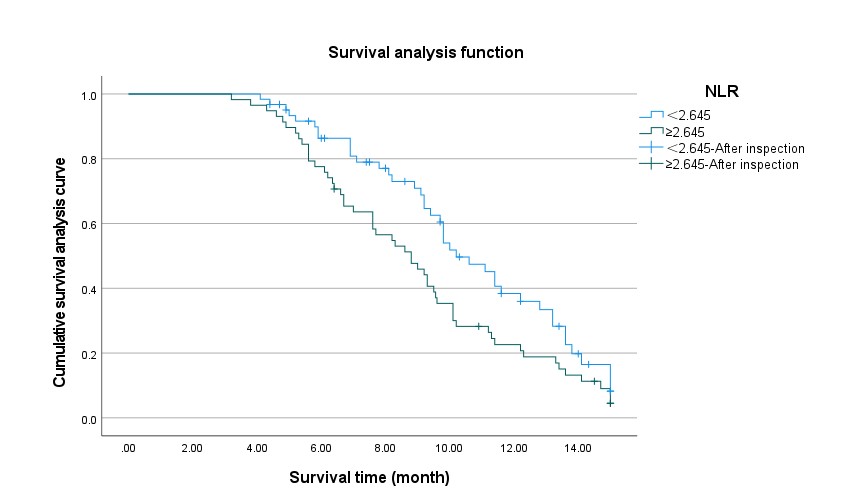
According to the expression of CD133 and CD44 in cancer tissues of NSCLC patients, they were divided into CD133 high expression group, CD133 low expression group, CD44 high expression group and CD44 low expression group. All NSCLC patients obtained 2-year follow-up data. The results showed that the median total survival time of the NLR low expression group was 10.2 months, significantly higher than that of the NLR high expression group by 8.8 months (X2 =4.650, P < 0.05), as shown in the following figure (Figure c); The median total survival time (OS) of CD44 high expression group was lower than that of low expression group, with OS of 9.3 months and 10.1 months, respectively (X²= 5.320, P < 0.05), as shown in Figure a; The median OS of CD133 high expression group was 9.2 months, while the median OS of CD133 low expression group was 12.8 months. The survival difference between the two groups was significant (X²= 5.829, P < 0.05), as shown in Figure b.
Discussion
In recent years, studies at home and abroad have reported that the existence of stem cells is the main cause of tumor metastasis and recurrence. Stem cells are a group of cell subsets with self-renewal, differentiation and passage ability. These cells have been found and confirmed to exist in many blood tumors and solid tumors, such as leukemia, prostate cancer, breast cancer and head and neck tumors. In basic experiments and clinical studies, these cells showed tolerance to traditional therapies, including surgery, radiotherapy and chemotherapy. The identification of tumor stem cell biomarkers may help to develop individualized chemotherapy drugs for tumor stem cell targeted therapy [20-24]. The cell-mediated inflammatory reaction plays an important role in carcinogenesis (which can be expressed as lymphocytes, neutrophils and monocytes in the whole blood cell count), so the ratio of neutrophils to lymphocytes (NLR) is a widely used prognostic marker for various tumors [25-27]. High NLR at baseline or during treatment is associated with poor prognosis, such as short overall survival (OS), short progression-free survival (PFS), or lack of response to treatment for lung cancer, colorectal cancer, renal cancer, and many other solid cancers. NLR is more likely to exist in patients with increased risk of cancer recurrence or poor postoperative results, and NLR is a more effective OS predictor than neutrophil count or lymphocyte count alone.
The results showed that CD44 and CD133 were positively expressed in NSCLC cancer tissues, while lymphocytes in peripheral blood were significantly reduced and neutrophils were significantly increased; Further analysis showed that the lower the degree of differentiation of NSCLC patients, the higher the positive expression of CD44 and CD133 protein in patients with lymph node metastasis. It was preliminarily suggested that the expression of CD44 and CD133 was closely related to the pathological characteristics of NSCLC patients. CD133 has been found overexpressed in many tumors, and is the most common marker to label tumor stem cells, such as ovarian cancer, breast cancer, and melanoma. CD133+cells have obvious characteristics of in vitro sphericity, tumo- rigenicity, cell differentiation and chemoresistance. CD44 expression is also very widespread, especially in stem cells, showing high expression. It is mainly involved in the adhesion between cell-cell and cell-matrix, and mediates multiple functions of cells including growth, differentiation and death. It is also another common marker of tumor stem cells; It is reported that CD44 is closely related to the poor prognosis of many kinds of cancer patients, and leads to tumor metastasis and chemotherapy resistance. This study indirectly explained that CD133 and CD44 were involved in the occurrence and development of NSCLC, and provided reference basis for NSCLC patients to study new anticancer drugs. In addition, the results of this analysis showed that the NLR of NSCLC patients with tumor size>3 cm and lymph node metastasis was significantly higher than that of other groups, indicating that the tumor size and lymph node metastasis of NSCLC were correlated with NLR. The higher the NLR value, the less lymphocytes in the patient's peripheral blood and the more neutrophils. The increase of neutrophils will damage the DNA of precancerous lesion cells by secreting reactive oxygen species, and produce vascular growth factor, which will promote the formation of tumor. By promoting the secretion of matrix meta- lloproteinases, it damages the extracellular matrix and interferes with the response of T cells. Lymphocytes can produce a series of cytotoxic factors. Inhibition and killing of tumor cells through multiple ways means that the inhibition of tumor cells is weakened. Therefore, NLR is closely related to the pathological characteristics of tumor patients.
The study found that the expression of CD133 was closely related to the occurrence, progression and prognosis of the disease. Therefore, CD44 and CD133 can be used as effective indicators for clinical evaluation of biological behavior and prognosis of non-small cell lung cancer. In addition, our study confirmed that NLR plays an important role in the occurrence and prognosis of NSCLC patients. The results of this analysis showed that the median total survival time of 10.2 months in the low NLR group was significantly higher than 8.8 months in the high NLR group (χ2=4.650, P<0.05), with statistical significance; The median total survival time (OS) of CD44 high expression group was lower than that of low expression group, with OS of 9.3 months and 10.1 months, respectively (χ2= 5.320, P<0.05); The median OS of CD133 high expression group was 9.2 months, and the median OS of CD133 low expression group was 12.8 months. The total survival time between the two groups was significantly different (χ2= 5.829, P<0.05) This confirms that the prognosis of NSCLC patients is closely related to the expression of CD44, CD133 and NLR, and further research is needed in the future. Therefore, we can preliminarily determine that the expression of CD44, CD133 and NLR is related to the pathological characteristics and prognosis of NSCLC patients, or provide a reference for clinicians to evaluate the prognosis and clinical treatment of patients, and provide theoretical basis for the individualized treatment and prolonging survival of patients with advanced non-small cell lung cancer.
Disclosure Statement
No potential conflict of interest was reported by the author(s).
Funding
This work was supported by Clinical Medical Technology Innovation Guidance Project of Hunan Provincial Science and Technology Department (2020- SK52003), National Science Foundation of Health and Family Planning Commission of Guizhou Province (gzwkj2022-472).
Availability of Data and Materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request
Ethics Approval and Consent to Participate
Written informed consent was obtained from all patients included in the present study, and this study was approved by the Ethics Committee of Shaoyang Central Hospital.
- Ferlay J, Colombet M, Soerjomataram I et al. (2019) Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int. J. Cancer 144: 1941-53.
- Shin JY, Yoon JK, Marwaha G (2018) Progress in the treatment and outcomes for early-stage non-small cell lung cancer. Lung 196: 351-8.
- Guan Y, Yang J, Liu X, Chu L (2020) Long noncoding RNA CBR3 antisense RNA 1 promotes the aggressive phenotypes of non-small-cell lung cancer by sponging microRNA-509-3p and competitively upregulating HDAC9 expression. Oncol Rep 44: 1403-14.
- Yoh K, Hosomi Y, Kasahara K et al. (2016) A randomized,double-blind, phase II study of ramucirumab plus docetaxel vs. placebo plus docetaxel in Japanese patients with stage IV non-small cell lung cancer after disease progression on platinum-based therapy. Lung Cancer 99: 186-93.
- Chen H, Shien K, Suzawa K et al. (2017) Elacridar, a third-generation ABCB1 inhibitor, overcomes resistance to docetaxel in non-small cell lung cancer. Oncol Lett 14: 4349-54
- . Shen HT, Chien PJ, Chen SH et al. (2020) BMI1-Mediated Pemetrexed Resistance in Non-Small Cell Lung Cancer Cells Is Associated with Increased SP1 Activation and Cancer Stemness. Cancers (Basel) 12: 2069.
- Crino L, Weder W, van Meerbeeck J, Felip E, Group EGW (2010) Early stage and locally advanced (non-metastatic) non-small-cell lung cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol 21: 103-15
- Feng YH, Su YC, Lin SF et al. (2019) Oct4 upregulates osteopontin via Egr1 and is associated with poor outcome in human lung cancer. BMC Cancer 19: 791.
- Tan BT, Park CY, Ailles LE et al. (2006) The cancer stem cell hypothesis: a work in progress. Lab Investig 86: 1203-7.
- Hardavella G, George R, Sethi T (2016) Lung cancer stem cells-characteristics, phenotype. Transl Lung Cancer Res 5: 272-9.
- Feng YH, Su YC, Lin SF et al. (2019) Oct4 upregulates osteopontin via Egr1 and is associated with poor outcome in human lung cancer. BMC Cancer 19: 791.
- . Varillas JI, Zhang J, Chen K et al. (2019) Microfluidic Isolation of Circulating Tumor Cells and Cancer Stem-Like Cells from Patients with Pancreatic Ductal Adeno carcinoma. [J]. Theranostics 9: 1417-25.
- Zhou S, Peng J, Xiao L et al. (2021) TRIM25 regulates oxaliplatin resistance in colorectal cancer by promoting EZH2 stability. Cell Death Dis 12: 463.
- Choi HS, Kim JH, Kim SL et al. (2019) Disruption of the NF-κB/IL-8 Signaling Axis by Sulconazole Inhibits Human Breast Cancer Stem Cell Formation. Cells 8: 1007.
- Powell D, Lou M, Barros Becker F et al. (2018) Cxcr1 mediates recruitment of neutrophils and supports proliferation of tumor-initiating astrocytes in vivo. Sci Rep 8: 13285.
- Coffelt SB, Wellenstein MD, Visser KE (2016) Neutrophils in cancer: neutral no more. Nature reviews. Cancer 16: 431-46.
- Ocana A, Nieto-Jimenez C, Pandiella A et al. (2017) Neutrophils in cancer: prognostic role and therapeutic strategies. Mol Cancer 16: 137.
- Dionísio MR, Vieira AF, Carvalho R et al. (2020) BR-BCSC Signature: The Cancer Stem Cell Profile Enriched in Brain Metastases that Predicts a Worse Prognosis in Lymph Node-Positive Breast Cancer. Cells 9: 2442.
- Cha YJ, Park EJ, Baik SH et al. (2019) Clinical significance of tumor-infiltrating lymphocytes and neutrophil-to-lymphocyte ratio in patients with stage III colon cancer who underwent surgery followed by FOLFOX chemotherapy. Sci Rep 9: 11617.
- Hu W, Zhao Y, Su L et al. (2021) Silencing the lncRNA NORAD inhibits EMT of head and neck squamous cell carcinoma stem cells via miR-26a-5p. Mol Med Rep 24: 743.
- Chang JC (2016) Cancer stem cells: Role in tumor growth, recurrence, metastasis, and treatment resistance. Medicine (Baltimore) 95: S20-5.
- Zhou H, Xu R (2015) Leukemia stem cells: The root of chronic myeloid leukemia. Protein Cell 6: 403-12.
- Leão R, Domingos C, Figueiredo A et al. (2017) Cancer Stem Cells in Prostate Cancer: Implications for Targeted Therapy. Urol Int 99: 125-36.
- Curtarelli RB, Gonçalves JM, Dos Santos LGP et al. (2018) Expression of Cancer Stem Cell Biomarkers in Human Head and Neck Carcinomas: A Systematic Review. Stem Cell Rev Rep 14: 769-84.
- Ayers KL, Ma M, Debussche G et al. (2021) A composite biomarker of neutrophil-lymphocyte ratio and hemoglobin level correlates with clinical response to PD-1 and PD-L1 inhibitors in advanced non-small cell lung cancers. BMC Cancer 21: 441.
- Farolfi A, Scarpi E, Greco F et al. (2020) Inflammatory indexes as predictive factors for platinum sensitivity and as prognostic factors in recurrent epithelial ovarian cancer patients: a MITO24 retrospective study. Sci Rep 10: 18190
- Wang F, Li P, Li FS (2019) Prognostic role of C-reactive protein to albumin ratio in colorectal cancer: A meta-analysis. Medicine (Baltimore) 98: e16064.

Tables at a glance
Figures at a glance