The Beta-thalassemic Child: Preventive and Therapeutic Approach in Odontostomatology - Two Clinical Case Reports
Received Date: December 28, 2024 Accepted Date: January 28, 2025 Published Date: January 31, 2025
doi: 10.17303/jdoh.2025.12.101
Citation: El Omari Fz, Faid K, Saih H, Bousfiha B, Benyahya I (2025) The Beta-thalassemic Child: Preventive and Therapeutic Approach in Odontostomatology - Two Clinical Case Reports. J Dent Oral Health 12: 1-8
Abstract
Thalassemia is a genetic blood disorder that disrupts hemoglobin production, resulting in chronic anemia. It is most common in regions such as the Mediterranean, the Middle East and South Asia. Severe forms, such as beta-thalassemia major, often require lifelong blood transfusions and treatment with iron chelation. In addition to the medical challenges, thalassemia can also have significant oral health implications, often requiring specialized dental care. This article highlights two clinical cases of patients with beta-thalassemia major who sought oral treatment, illustrating the unique considerations for managing their dental needs alongside their systemic condition.
Keywords: Thalassemia; Preventive Care; Oral Care; Pediatric Dentistry
Introduction
Thalassaemia is a quantitative abnormality of haemoglobin caused by mutations in genes controlling the production of beta globins, primarily classified into alpha-thalassemia (α-thalassemia) and beta-thalassemia (β-thalassemia) [1]. These hemoglobinopathies are widespread in the Mediterranean basin, Middle East, asia [2]. Βeta-thalassemia is the most commonly found variety of thalassemia that affects approximately 60 to 80 million individuals in the world, and approximately 3% of the total population around the world is carrying the β thalassemia gene [3]. The annual numbers of expected newborns with β‐thalassemia are 20 420 in Southeast Asia, 9914 in the Eastern Mediterranean region, 1019 in Europe, and 341 in North, Central, and South Americas [4].
Thalassemia Major (TM) is the major form of the disease that causes severe anemia, leading to several medical problems, such as growth and facial deformities [3,5-8]. The treatment of thalassemia is based on blood transfusions combined with iron chelation therapy [9,10]. Thalassemia and its treatment have a major impact on maxillofacial and alveolar growth, as well as on dental organogenesis, requiring special management [3].
Case Report
Case 1
The patient M. was a 9 years old girl who suffered from Thalassemia major. She was referred by her doctor for oral cavity repair. The ongoing treatment for that patient was transfusion once a month associated with iron-chelation therapy with deferiprone (Ferriprox®).
This patient showed general symptoms such as anemia, pallor, jaundice, stunted growth and development, and hepatosplenomegaly. Additionally, maxillofacial features included a characteristic of ‘’asian facies’’ appearance (Figure 1).
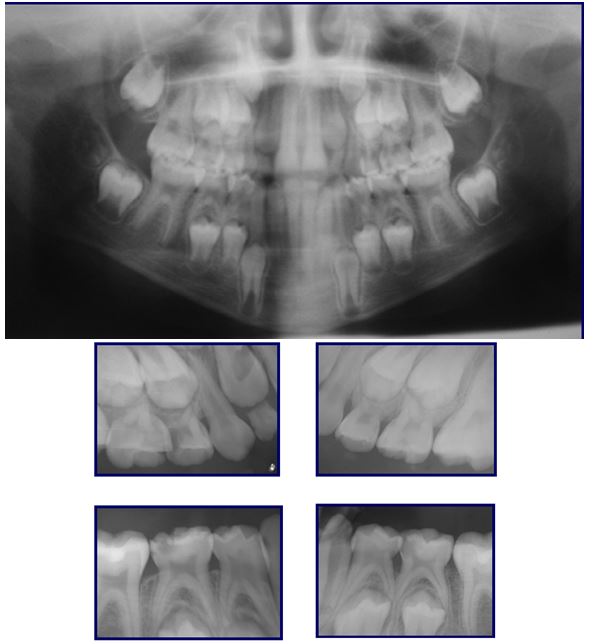
The clinical examination of the oral cavity revealed several notable findings. The mucosa showed pallor with papillary atrophy. There was a delayed tooth eruption, as well as enamel and dentin defects. In addition, multiple caries were observed and the patient presented a Class 2 molar relationship. (Figure2) Dental radiography showed the presence of dentino-pulpal damage on tooth 54 and 85, dentinal caries on tooth 65 and 75, and superficial caries on the four first permanent molars (Figure 3).
The first step in managing this patient was to request a blood test that included NFS, TS, prothombin and platelet levels, in order to evaluate the risk of infection and bleeding. Therefore, the precaution taken in this case to control bleeding was to provide local hemostasis tools like compression, hemostatic products, etc. For surgical procedures like extractions, an antiobioprophylaxis was prescribed before the act to prevent from the risk of infection.
We decided for this case to opt for a radical treatment concerning tooth 54 and 75, which consisted in the extraction of both of them. Concerning tooth 85 and 55, dental restorations were performed. As for the first permanent molars, preventive care was established with a regular follow-up (Figure4).
Case 2
The patient O. was a 9 years old girl who suffered from Thalassemia major. He was referred by his doctor for having a dental infection that caused a parulic abscess. The ongoing treatment for that patient was similar to the first one : transfusion once a month associated with iron-chelation therapy with deferiprone (Ferriprox®).
This patient showed general symptoms such as anemia, pallor, jaundice, stunted growth and development, and hepatosplenomegaly. As for maxillofacial features, they included a characteristic of ‘’asian facies’’ appearance associated with excessive overhang (Figure 5).
The clinical examination of the oral cavity revealed several notable findings. The mucosa showed paleness with papillary atrophy. There were some caries with a parulic abscess related to tooth 85 (Figure 6).
Like we did for the patient in the first case, the first step in managing this patient was to request a blood test, in order to evaluate the risk of infection and bleeding. The same precautions were taken including antiobiotic prohpylaxis and local hemostasis. The source of infection was eradicated in the first place by extracting tooth 85. Then preventive care was applied for the first permanent molars, with a regular follow-up for the patient (Figure 7).
Discussion
Clinical manifestations in thalassemia patients differ varying from minor morphologic abnormalities to life threatening conditions [3]. Individuals with β-thalassemia major may present with the following general symptoms: pallor due to severe anemia, poor weight gain, delayed growth, mild jaundice, and hepatosplenomegaly [10,11]. Feeding problems, diarrhea, irritability, and recurrent bouts of fever may occur, as well as cardiac, hepatic and endocrine complications [11]. In addition, β-thalassemia major leads to characteristic skeletal changes due to ineffective erythropoiesis in affected patients [5,11]. Maxillofacial symptoms of β-thalassemia major include hyperplasia of the facial bones, leading to an ‘’Asian-like’’ appearance [10,12]. Other features include reduced thickness of the inferior mandibular cortex, decreased overall bone density due to bone marrow overgrowth, thinning of the cortical bone, absence of the inferior alveolar canal, smaller maxillary sinuses, and generalized osteoporosis [10,13,14].
Patients with β-thalassemia major often present with various oral and dental abnormalities. Occlusal disorders include maxillary proalveolus, dental and skeletal Class II malocclusion, excessive anterior open bite, horizontal overjet and various positional anomalies [10,12,13]. In addition, organogenesis disorders are commonly observed, such as delayed tooth eruption, enamel and dentin defects, pulpal calcifications, and disturbances in root development [10,12,15]. There are also other oral symptoms related to anemia in these patients, which include pale skin and mucous membranes, bilateral angular cheilitis, glossitis, tongue edema and papillary atrophy [10,15]. All these factors contribute to an increased caries risk and significant periodontal involvement in these patients [10].
The therapeutic approach for these patients is divided into two aspects: a preventive approach and a therapeutic approach. These patients suffer from severe anemia, hemolysis and ineffective erythropoiesis and possible diabetes, treatments including transfusions, splenectomy, iron chelation therapy, central venous catheters and stem cell transplantation further contribute to a greater risk of infection [16].
In order to minimize the risk of infection and bleeding in thalassemia patients, the clinician needs to contact the referring doctor to clarify the specific type of thalassemia, current treatments and any concomitant pathologies. Preoperative blood tests, including TS, prothrombin time and palatelet levels should be requested [7,15]. The invasive procedures should be performed in the week following the transfusion, after antibiotic prophylaxis and coagulation studies. The level of hemoglobin must be higher than 110 g/l before any clinical procedure [16]. Local hemostasis should be ensured using hemostasic products, and antibiotic prohylaxis should be prescribed one hour before surgical procedures, such as endodontic treatments or extractions in order to prevent infection [7,15]. Regarding the therapeutic approach, it involves eradicating sources of infection by taking precautions tailored to each situation [15]. If the pulp is affected, temporary teeth should undergo appropriate treatment, while permanent teeth may require endodontic treatment for simple root canal anatomy. Oral care should be prioritized, especially in splenectomized patients, who may need radical dental procedures for pulpal involvement in both temporary and permanent teeth [7,17]. Additionally, penicillin, commonly used in these patients, should be avoided when possible due to potential antibio-resistance [17].
Conclusion
The risk of developing various oral and dental diseases in thalassemic patients is very high. Thus, preventive measures must be taken against these oral diseases and are therefore considered very important as it increases an individual’s wellbeing and also helps in higher life expectancy among these patients. The dentist, especially a specialist pediatric dentist, plays a crucial role in educating thalassemic patients and their parents or caregivers with regards to preventing dental caries and regarding the importance of maintenance of good and adequate oral hygiene status.
- Roussos P, Mitsea A, Halazonetis D, Sifakakis I (2021) Craniofacial shape in patients with beta thalassaemia: a geometric morphometric analysis. Sci Rep. 11: 1686.
- Noori T, Ghazisaeedi M, Aliabad GM, Mehdipour Y, Mehraeen E, Conte R, Safdari R (2019) International Comparison of Thalassemia Registries: Challenges and Opportunities. Acta Inform Med. 27: 58-63.
- Nabi Aaysha T, Muttu Jayalakshmi, Chhaparwal Amit, Mukhopadhyay Arka, Pattnaik Samarjeet J, Choudhary Pallawee (2022) Implications of β-thalassemia on oral health status in patients: A cross-sectional study. Journal of Family Medicine and Primary Care, 11: 1174-8.
- Kattamis A, Forni GL, Aydinok Y, Viprakasit V (2020) Changing patterns in the epidemiology of β-thalassemia. Eur J Haematol. 105: 692-703.
- Abbasi F, Tabesh A, Yavari A, Makaremi R, Bizhani O, Mahmood M (2023) Evaluation and relation of oral health-related quality of life and oral health status in Thalassemia Major patients, a cross-sectional study. BMC Oral Health. 23: 493.
- Millot S, WoimantH, EjeilAL , Charrier JL (2011) About a case of β-thalassemia: new implications of this pathology and its treatments in oral surgery. EDP Sciences.
- Helmi N, Bashir M, Shireen A, Ahmed IM (2017) Thalassemia review: features, dental considerations and management. Electron Physician, 9: 4003-8.
- Amirabadi F, Saravani S, Miri-Aliabad G, Khorashadi- Zadeh M (2019) The Association between Dental Health Status and Oral Health-Related Quality of Life of Children Diagnosed with beta-Thalassemia Major in Zahedan City, Iran. Int J Pediatr. 7: 8985-91.
- Biffi A (2018) Gene Therapy as a Curative Option for β-Thalassemia. N Engl J Med. 378: 1551-2.
- Cappellini MD, Cohen A, Porter J, Taher A, Viprakasit V, eds. (2014) Guidelines for the Management of Transfusion Dependent Thalassaemia (TDT). 3rd ed. Nicosia (CY): Thalassaemia International Federation.
- Langer AL, Adam MP, Feldman J, Mirzaa GM, Pagon RA, Wallace SE, Amemiya A, eds (2000) GeneReviews®. Seattle (WA): University of Washington.
- Gupta DK, Singh SP, Utreja A, Verma S (2016) Prevalence of malocclusion and assessment of treatment needs in β-thalassemia major children. Prog Orthod. 17: 7.
- Tabesh A, Abbasi F, Shavakhi M, Mahmood M (2022) Oral health related quality of life and orthodontic treatment need in thalassemia major patients. Dent Res J. 19: 70.
- Bayati S, Keikhaei B, Bahadoram M, Mahmoudian-Sani MR, Vaneshani M, Behbahani F (2021) Radiographic Features of the Maxillofacial Anomalies in Beta-Thalassemia Major: With New View. World J Plast Surg. 10: 78-83.
- Mulimani P, Abas AB, Karanth L, Colombatti R, Kulkarni P (2023) Treatment of dental and orthodontic complications in thalassaemia. Cochrane Database Syst Rev. 2: CD012969.
- Labrini F, Oubenyahya H (2018) Dental Management of Beta Thalassemia Major patients: A Review. International Journal of Medicine & Health Research. 4: 1-5
- Millot S, Woimant H, Ejeil AL, Charrier JL (2011) Beta thalassemia major: update of treatment in oral medicine. Med Oral Surgery Oral, 17: 51-4.







Figures at a glance