Estimation of the Level of Salivary Flow among Yemeni Khat Chewers Compared to Non-Chewers
Received Date: December 31, 2024 Accepted Date: January 31, 2025 Published Date: February 03, 2025
doi: 10.17303/jdoh.2025.12.102
Citation: Mohammed Bin Taja, Baleegh Al-kadasi, Manal Al-Hajri, Salah Hafedh, Saeed Saeed, et al. (2025) Estimation of the Level of Salivary Flow among Yemeni Khat Chewers Compared to Non-Chewers. J Dent Oral Health 12: 1-10
Abstract
Background and Objectives: A lot of studies have referred to the correlation between Khat chewing and xerostomia but this is the first time to use sialometry in measuring both Clinical Oral Dryness Score (CODS) and salivary flow rate (SFR) to define that correlation. No doubt to that correlation, the updating and follow-up of information regarding that correlation using simple and more accurate method is needed which is provided by this study. The aim of this study was to estimate level of salivary flow rate among Yemeni Khat chewers and comparing that with non-Khat chewers.
Material and Method: A case control study survey was conducted to determine the prevalence of Xerostomia among a sample of Yemeni Khat chewers of population at labor age through clinical observation, questionnaires and direct measuring of salivary flow using sialometry. The sample size was 200 random patients selected from the cases in dental clinics of Sana'a University during July 2019 to December 2021. The studied population were between 16-50 years old. We divided the approved population into two groups: Group 1 which is the study group composed of Khat chewers and Group 2 which is the control group composed of non-Khat chewers. All statistical analysis were performed using the statistical Package for Social Science (SPSS) version 24.XVIII
Result: 171 (85.5%) of the subjects were Khat chewers with 125 (62.5%) of the subjects are daily consumers. 29 (14.5%) of the subjects were non Khat chewers at all. The studied population was of 74.0% male and 26.0% female with ages of population at labor age ranging like following:
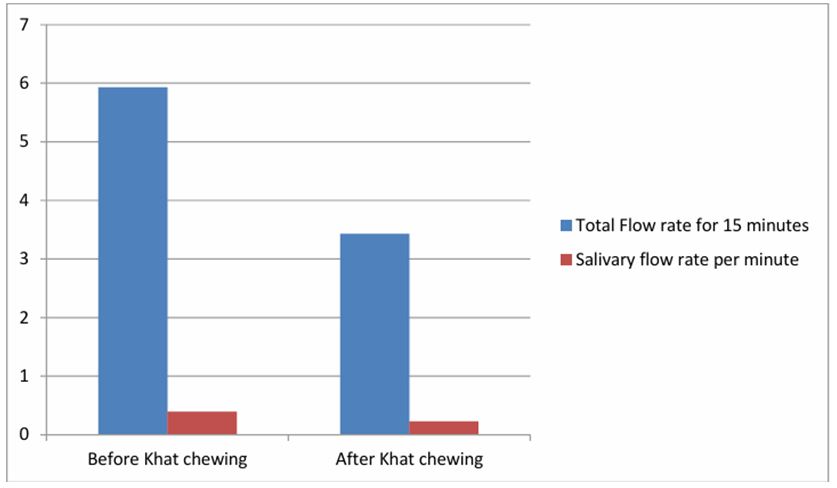
15 – 20 years (10.5%), 21 – 25 years (54.5%), 26 – 30 years (10.0%), 31 – 35 years (15.5%) and 36-50 years (9.5%). In general, 23 (12.3%) of the subjects said that their mouth always feels dry when eating a meal. Khat chewing objects showed a decline in total SFR before chewing Khat in compare to control group. The mean SFR for Khat chewing objects before chewing Khat was 5.80 milliliter (mL) in compare to those who don't chew Khat where their SFR was 6.67 mL. After chewing Khat, the mean SFR for objects was 3.45 mL showing a decline of 2.35 mL. The mean of total SFR per minutes decreases after Khat chewing. Before Khat chewing, the mean of total SFR for 15 minutes was 5.93 mL with SFR per minute equal to 0.395mL. After Khat chewing, the mean of total SFR for 15 minutes was 3.43 mL with SFR per minute equal to 0.229 mL.
Conclusion: The prevalence of xerostomia in Yemen labor force in general is 16.33% and after Khat chewing is 56.93%. Khat chewing increase the occurrence of xerostomia by 40.6% among Yemeni labor Khat chewers and the prevalence of Khat chewing habit is 85.5% with 62.5% regarded as daily consumers of Khat which indicates high increase in Khat daily consumers.
Keywords: Orthodontics; Periodontology; Oral Medicine; Oral Surgery; Khat Chewers; Xerostomia
Introduction
Khat (Catha edulis) is a green shrub native to East Africa and Yemen, where its leaves are commonly chewed for their stimulant effects. Khat chewing has a long history among the Yemeni people and is a widespread social habit in the region. In addition to Yemen, Khat is also grown and consumed in parts of East Africa, including Ethiopia, Somalia, Djibouti, Eritrea, Kenya, Madagascar, and Tanzania (Numan et al., 2012). The primary psychoactive compounds in Khat are cathinone and cathine, which are structurally similar to amphetamine and produce moderate euphoria and excitation when chewed [1,2]. Prolonged Khat chewing has been associated with various systemic health effects, including cardiovascular diseases, gastrointestinal disorders, liver and renal toxicity, as well as psychological and mental disturbances [3]. Regarding oral health, Khat chewing has been reported to have harmful effects on dental and oral tissues, such as keratotic white lesions, mucosal pigmentations, plasma cell stomatitis, teeth attrition and discoloration, gingival recession, and xerostomia (dry mouth) [4-6].
Xerostomia is a disorder related to hyposecretion of saliva, which plays an essential role in maintaining optimal oral health by managing lubrication, pH, cleanliness, and integrity of the oral cavity and mucosa [7,8]. Untreated xerostomia can lead to a decrease in oral pH, increased plaque formation, and dental caries, as well as oral candidiasis [8]. The association between Khat chewing and xerostomia has been well documented in the literature [5,9,10]. However, according to the archive of the National Information Center in Yemen, there is no study in Yemen that has investigated xerostomia using sialometry, a relatively common procedure in clinical practice that involves measuring salivary flow rate (SFR). This study aims to evaluate and estimate salivary flow rate among Yemeni Khat chewers of the population at labor age (16-50 years) in comparison with non-chewers. Specific objectives include determining the presence of mouth dryness among Yemeni people, assessing the correlation between Khat chewing and salivary flow rate, and updating the information related to the prevalence of xerostomia in Yemen.
Literature Review
Saliva: Definition, Composition, and Functions
Saliva is a clear, watery, viscous fluid with a pH of 6-7, secreted by the parotid, submandibular, sublingual, and minor salivary glands of the oral cavity [8]. It is composed of fluid ions (potassium, bicarbonate, sodium, and chloride) and both serous and mucous proteins [8]. Saliva plays an essential role in maintaining optimal oral health, acting as an antimicrobial constituent, lubricating the oral cavity and mucosa, managing pH, and maintaining cleanliness and integrity [7,8]. Saliva is produced by the major (parotid, submandibular, and sublingual) and minor salivary glands, with the major glands contributing approximately 93% of the total saliva volume and the minor glands contributing the remaining 7% [11]. Saliva production is a two-stage process: first, active secretion of salts (sodium and chloride) in the acinar cells, followed by modification of the primary fluid by the ducts through the removal of sodium and chloride and the addition of potassium and bicarbonate (Turner, 2007). Salivary components, such as amylase, mucins, lysozyme, lactoferrin, and immunoglobulins, play various protective and functional roles in the oral cavity. Amylase is involved in the conversion of starch to maltose, while lysozyme and lactoferrin have antibacterial properties [12]. Mucins contribute to lubrication and protection of the oral mucosa, and secretory IgA helps aggregate bacteria and neutralize toxins (McNabb and Tomasi, 1981).
Salivary Flow Rate
Saliva is produced in both resting (unstimulated) and stimulated forms. Resting saliva is primarily secreted from the basal area under the tongue to lubricate the oral tissues, while stimulated saliva is generated from all areas of the mouth during muscular activity or olfactory stimulus [12]. The index used to measure the level of salivation is called salivary flow (SF), which can be categorized as unstimulated (u-SFR) or stimulated (s-SFR) (da Silva Marques et al., 2011). Hyposalivation, or a measurable decrease in salivary flow, can lead to xerostomia, the subjective sensation of oral dryness. Xerostomia can also occur without hyposalivation (Nederfors et al., 2000). The normal range for unstimulated salivary flow rate is 0.25-0.35 mL/min, and for stimulated salivary flow rate, it is 1-3 mL/min (da Silva Marques et al., 2011). Hyposalivation is defined as an unstimulated salivary flow rate of less than 0.1 mL/min and a stimulated salivary flow rate of less than 0.7 mL/min (Ship et al., 1999).
Khat: Taxonomy, Chemical Composition, and Effects
Khat (Catha edulis) is a green shrub that grows in the Khat belt, stretching from eastern to southern Africa and the western part of the Arabian Peninsula. The plant's leaves contain the psychoactive compounds cathinone and cathine, which are structurally similar to amphetamine and responsible for the stimulant effects experienced by Khat users [13].
When Khat is consumed, the active chemicals break down into cathine and norephedrine, as well as [R,S-norephedrine] and [R,R-norpseudoephedrine], which are structurally similar to amphetamine [14]. The use of Khat is associated with various health effects, including hyperthermia, euphoria, increased respiration and sensory stimulation, excitement, anorexia, violent behavior, schizophrenia, paranoia, psychosis, elevated blood pressure, insomnia, tachycardia, irritability, migraine, and sexual dysfunction (Lo Faro et al., 2020). Khat chewing is a common social and cultural activity in Yemen, often practiced in group settings. The habit typically involves chewing the fresh Khat leaves and keeping the chewed material in the buccal sulcus for several hours, either unilaterally or bilaterally, before expectoration [15]. Reasons for Khat chewing include social interaction, the belief that it enhances contact with Allah during prayer, and the perceived enhancement of cognitive and physical abilities [1,16].
Khat Chewing and Oral Health
Khat chewing has been associated with various oral and dental disorders, including periodontal diseases, dental caries, temporomandibular joint disorders, plasma cell stomatitis, mucosal pigmentation, keratotic lesions, and xerostomia [6,17,18]. The association between Khat chewing and xerostomia has been well documented. Several studies have reported that Khat chewers experience oral dryness, which is believed to be due to the amphetamine-like effect of Khat, salivary gland fatigue from continuous chewing, or the metabolic effects of Khat on salivary acini tissues [9,10,19].
Xerostomia: Definition, Causes, and Complications
Xerostomia, or the sensation of having a dry mouth, is one of the most prevalent complaints among the elderly, with prevalence rates ranging from 10% to 40% in individuals over the age of 50 (Matear et al., 2005). Xerostomia can result from various causes, including factors affecting the salivary center (e.g., psychological problems, neurological disorders), alterations in nerve stimulation of saliva (e.g., dehydration, smoking, medications), and changes in salivary gland function (e.g., obstruction, infection, autoimmune diseases, radiation therapy) [20,21]. Medications are a common cause of xerostomia, as over 400 drugs, many of them in common use, can induce salivary gland hypofunction (Sreebny et al., 1997; Kim YJ, 2023). Chronic disorders such as diabetes and Sjögren's syndrome have also been linked to hyposalivation and xerostomia (Ohara et al., 2016; Åstrøm et al., 2019). If left untreated, xerostomia can decrease oral pH, leading to increased plaque formation and dental caries, as well as oral candidiasis (Bartels, 2014; Ship et al., 1999; Turner et al., 2007). Patients with xerostomia may experience difficulties with speaking, chewing, swallowing, and wearing dentures [22].
Sialometry, the measurement of salivary flow rate, is a relatively common procedure in normal clinical practice and is considered the most accurate and available method to diagnose xerostomia and evaluate salivary gland function [21]. Sialometry involves measuring the unstimulated salivary flow rate (u-SFR) and stimulated salivary flow rate (s-SFR), as well as other parameters such as palatal secretion (PAL) and parotid secretion (PAR) (Ship et al., 1999).
Very low unstimulated and stimulated salivary flow rates, or hyposalivation, are defined as less than 0.1 mL/min and less than 0.7 mL/min, respectively (Ship et al., 1999). Sialometry is essential in distinguishing between true xerostomia (Xerostomia Vera, primaria), caused by salivary gland malfunction, and pseudo-xerostomia (Xerostomia Spuria, symptomatica), which is the subjective sensation of oral dryness despite normal salivary gland function (Ship et al., 1999).
Study Design and Population
This case-control study was conducted to determine the prevalence of xerostomia among a sample of Yemeni Khat chewers of the population at labor age (16-50 years) through clinical oral dryness score, questionnaires, and direct measurement of salivary flow using sialometry. The study was carried out in Sana'a city, and the target population was 200 patients selected from the cases at the teaching hospital of Sana'a University during July 2019 to December 2021. The participants were divided into two groups: Group 1 (the study group) comprised Khat chewers, and Group 2 (the control group) comprised non-Khat chewers.
Inclusion and Exclusion Criteria
The inclusion criteria were:
- Khat chewers of both male and female dental patients should be aged 16-50 years old
- The participant should attend the dental clinics of Sana'a University during the study period.
- Patients who understood and voluntarily agreed to keep all the scheduled appointments for data collection.
- The participant should be healthy, and his salivary gland should be normal.
- The participant should not be smokers or alcoholic
The exclusion criteria were:
- Any participant who was not fit with inclusion criteria should be excluded
Data Collection
The study participants were given a patient information sheet and an informed consent form. A structured interview was conducted, including aspects related to the perception of dry mouth based on the Zero Xerostomia Questionnaire.
The questionnaire used by the examiner had three parts:
1. Basic information and dental and medical history to exclude subjects who did not match the research criteria.
2. Case sheets used to register the measurements taken by the researcher.
3. Chronic Oral Dryness Score (CODS) and modified xerostomia questionnaires.
Saliva Collection and Sialometry
Saliva collection was performed as follows:
- Environmental controls: Samples collected in a temperature regulated room (22-24 C)
-Timing standardized to morning hours to minimize circadian rhythm effects.
- Hydration status conformed via self-report participant fasted for 2 hours pre-test.
- The patient laid down in an upright position, and saliva was collected for five minutes with the head down, with the patient spitting the saliva into a graded tube without swallowing.
- The steps were repeated for another two five-minute periods, with a five-minute rest between collections.
- The same procedure was repeated the following morning after Khat chewing.
The mean of the total salivary flow rate for 15 minutes and the salivary flow rate per minute were calculated for each patient.
Statistical Analysis
Statistical analysis was performed using SPSS version 24. Frequency, distribution, and the chi-square test were used to investigate the significant differences in the prevalence of xerostomia between non-Khat chewers and Khat chewers. Welch's t-test was used to compare the significant differences between the mean values of xerostomia in both groups. Welch’s t-test was selected due to unequal variances and group sizes (non-chewers n =29 vs. chewers n= 171) , ensuring robustness against heteroscedasticity.
Results
Demographic Characteristics of the Study Population
The study population consisted of 200 individuals, with 148 males (74.0%) and 52 females (26.0%) Table (1). The mean age was 26.37 years, with the majority of subjects (54.5%) being 21-25 years old Table (2).
Prevalence of Khat Chewing Habit
Of the 200 subjects, 171 (85.5%) were Khat chewers, and 125 (62.5%) were daily consumers. Only 29 (14.5%) were non-Khat chewers (Table 3).
Salivary Flow Rate Measurements
The mean total salivary flow rate for 15 minutes was higher in the non-Khat chewers group (6.67 mL) compared to the Khat chewers group (5.80 mL) before Khat chewing. After Khat chewing, the mean total salivary flow rate for the Khat chewers group decreased to 3.45 mL, indicating a decline of 2.35 mL (Figure 1).
The mean salivary flow rate per minute also decreased after Khat chewing, from 0.395 mL/min before Khat chewing to 0.229 mL/min after Khat chewing. The longer the duration of Khat chewing, the lower the total salivary flow rate. Khat chewers who chewed for 4 hours or less had a mean total salivary flow rate of 6.18 mL before Khat chewing, compared to 5.25 mL for those who chewed for 8 hours or more.
Clinical Results Using Unstimulated Salivary Flow (USF)
The data from the 15-minute saliva collection period was divided into three Clinical Results Using Unstimulated Salivary Flow (USF)
The data from the 15-minute saliva collection period was divided into three 5-minute intervals to analyze the USF.
Before Khat chewing, the USF data showed:
- In the first 5-minute period, 13.0% had ≤1 mL, 22.0% had 1.1-1.5 mL, and 27.0% had 1.51-2.0 mL.
- In the second 5-minute period, 16.5% had ≤1 mL, 20.5% had 1.1-1.5 mL, and 27.5% had 1.51-2.0 mL.
- In the third 5-minute period, 19.5% had ≤1 mL, 21.5% had 1.1-1.5 mL, and 27.0% had 1.51-2.0 mL.
After Khat chewing, the USF data showed a significant increase in the proportion of subjects with ≤1 mL of USF, reaching over 50% in each 5-minute interval.
The mean USF per minute before Khat chewing was 0.395 mL/min, which decreased to 0.229 mL/min after Khat chewing, indicating hyposalivation.
When comparing the USF of Khat chewers and non-chewers, the mean USF was significantly lower in the Khat chewers group both before and after Khat chewing.
Results from the Chronic Oral Dryness Score (CODS)
The CODS questionnaire showed that 49.5% of the subjects had mild xerostomia (score 1-3), 45.5% had moderate xerostomia (score 4-6), and 5.0% had severe xerostomia (score 7-10) (table 4).
Comparison with Modified Xerostomia Questionnaire
The modified xerostomia questionnaire did not show a significant difference in the mean scores between Khat chewers (9.329) and non-chewers (9.519), with a p-value of 0.638.
Discussion
The current study aimed to evaluate and estimate salivary flow rate among Yemeni Khat chewers of the population at labor age in comparison with non-chewers. The findings demonstrate a clear association between Khat chewing and reduced salivary flow, with Khat chewers exhibiting significantly lower salivary flow rates compared to non-chewers.
The prevalence of xerostomia, as determined by the direct measurement of salivary flow rates, was 16.33% in the general Yemeni labor force and increased to 56.93% among Khat chewers after Khat consumption. This indicates that Khat chewing increases the prevalence of hyposalivation by 40.6%, underscoring the detrimental impact of this cultural practice on oral health. The results from the CODS questionnaire, however, showed a higher prevalence of xerostomia, with 49.5% of subjects experiencing mild xerostomia, 45.5% moderate xerostomia, and 5.0% severe xerostomia. In contrast, the modified xerostomia questionnaire did not reveal significant differences between Khat chewers and non-chewers. These findings suggest that the use of questionnaires, while convenient, may not accurately reflect the true prevalence of xerostomia compared to the more objective and reliable method of direct salivary flow measurement (sialometry). The discrepancy in results highlights the importance of utilizing sialometry as the gold standard for diagnosing and studying xerostomia, particularly in the context of Khat chewing.
The study also found that the longer the duration of Khat chewing, the lower the total salivary flow rate. This could be attributed to the limited absorption of Khat's active components in the gastrointestinal tract over time, as well as the potential fatigue of the masticatory muscles from prolonged chewing. Interestingly, the study did not find a significant difference in the impact of Khat chewing on salivary flow between males and females. This suggests that the effect of Khat on xerostomia is consistent across genders within the Yemeni labor force population. The findings of this study contribute to the limited research on xerostomia in Yemen and provide valuable insights into the relationship between Khat chewing and salivary gland function. The data generated can inform public health interventions and strategies aimed at addressing the oral health implications of this widespread cultural practice in Yemen.
The limitation of this study was the reliance on self-reported khat use, future studies should validate with biochemical markers the other limitation was the single-site recruitment limits generalizability, multi-center studies recommended.
Conclusion
This study demonstrates that Khat chewing has a significant negative impact on salivary flow among the Yemeni labor force population. The prevalence of xerostomia, as measured by direct salivary flow assessment, is substantially higher among Khat chewers compared to non-chewers. The results highlight the importance of utilizing sialometry as the primary method for diagnosing and studying xerostomia, as questionnaire-based approaches may not accurately reflect the true prevalence of this condition. Addressing the oral health implications of Khat chewing is crucial for improving the overall well-being of the Yemeni population. The findings of this study can guide the development of targeted interventions and educational campaigns to raise awareness about the risks of Khat chewing and promote oral hygiene practices among Yemeni citizens.
Policy Recommendations
1. Workplace partnership to educate laborers on khats oral and risks.
2. Integrate sialometry into routine dental screenings for khat users.
3. National campaigns to reduce khat dependence emphasizing oral health.
- Kalix P (1984) The pharmacology of khat. General Pharmacology: The Vascular System, 15: 179-87.
- Kalix P (1987) Khat: a plant with amphetamine effects. Journal of Substance Abuse Treatment, 4.
- Al-Motarreb A, Baker K, Broadley KJ (2002) Khat: pharmacological and medical aspects and its social use in Yemen. Phytotherapy Research, 16: 403-13.
- Al-Maweri SA, Alaizari NA, Al-Sufyani GA (2014) Oral mucosal lesions and their association with different risk factors among Al-Mukalla population, Yemen: a cross-sectional study. Journal of International Society of Preventive & Community Dentistry, 4: S84.
- Al-Sharabi AK (2002) Oral and para-oral lesions caused by takhzeen al-qat (khat chewing). The journal of the Bahrain Medical Society, 14: 70-4.
- Al-Sharabi AK, Shuga-Aldin H, Ghandour I, Al-Hebshi NN (2013) Qat chewing as an independent risk factor for periodontitis: a cross-sectional study. The International Journal of Dentistry.
- Del Vigna de Almeida P, Gregio AM, Machado MA, de Lima AA, Azevedo LR (2008) Saliva composition and functions: a comprehensive review. The Journal of Contemporary Dental Practice, 9: 072-80.
- Bartels C (2014) Salivary gland function. In Oral and Maxillofacial Surgery. 1213-35.
- Al-Alimi AR, Aguib HE, Warnakulasuriya S (2014) Khat (Catha edulis) chewing habit and its association with periodontal diseases (a systematic review and meta-analysis). International Journal of Dental Hygiene, 12: 165-72.
- Astatkie A, Demissie M, Berhane Y, Worku A (2015) Prevalence of and factors associated with regular khat chewing among university students in Ethiopia. Substance Abuse and Rehabilitation, 6: 41-50.
- Berkovitz BK, Moxham BJ, Linden RW (Eds.) (2011) Master Dentistry Volume 3 Oral Biology E-Book. Elsevier Health Sciences.
- Humphrey SP, Williamson RT (2001) A review of saliva: normal composition, flow, and function. The Journal of Prosthetic Dentistry, 85: 162-16.
- Feyissa AM, Kelly JP (2008) A review of the neuropharmacological properties of khat. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 32: 1147-66.
- Brenneisen R, Fisch HU, Koelbing U, Geisshüsler S, Kalix P (1990) Amphetamine-like effects in humans of the khat alkaloid cathinone. British Journal of Clinical Pharmacology, 30: 825-8.
- Ali AA (2007) Qat habit in Yemen society: a causative factor for oral periodontal diseases. International Journal of Environmental Health Research, 17: 213-23.
- Hassan NA, Gunaid AA, Murray-Lyon IM (2007) Khat (Catha edulis): health aspects of khat chewing. Eastern Mediterranean Health Journal, 13: 706-18.
- Hijazi MA, Hussein RA, Lila AM (2016) Takhzeen Al-Qat (Khat Chewing) Practice and Its Oral and General Health Impact: An Update. Open Journal of Stomatology, 6: 228-39.
- Al-Kholani AI (2010) Influence of khat chewing on periodontal tissues and oral hygiene status among Yemenis. Dental Research Journal, 7: 1-6.
- Al-Qadhi H, Al-Hebshi NN, Al-Bahrani B, Bashanfer S (2012) Impact of khat chewing on the whole unstimulated saliva and dental caries. International Journal of Dental Hygiene, 10: 51-5.
- DJ N, Bakutra G, Pandit P (2008) Xerostomia and its management. Contemporary Clinical Dentistry, 18: 212.
- Dost F, Farah CS (2013) Stimulated whole saliva flow rate and pH in patients with oral mucosal disease. Australian Dental Journal, 58: 519-24.
- Guggenheimer J, Moore PA (2003) Xerostomia: etiology, recognition and treatment. The Journal of the American Dental Association, 134: 61-9.

Tables at a glance
Figures at a glance