Daily Food Deprivation as a Predictor of in-Hospital Mortality with 75% Cutoff
Received Date: March 19, 2024 Accepted Date: April 19, 2024 Published Date: April 22, 2024
doi: 10.17303/jfn.2024.10.101
Citation: Hiroyo Miyata, Ayako Tsunou, Yoko Hokotachi, Teruyoshi Amagai (2024) Daily Food Deprivation as a Predictor of in-Hospital Mortality with 75% Cutoff. J Food Nutr 10: 1-13
Abstract
Objective: To examine the validity of once-a-year nutritional survey, a cross-sectional dietary survey conducted once a year is enough or not.
Methods: All hospitalized patients at a single institution admitted on the third Thursday of May, August, November and next February 2016 were enrolled and classified by admission style: emergency (group E) and scheduled (group C). Then, compared all data among four seasons whether the food intake in hospital impact on in-hospital mortality.
Results: 1. Mortality rate was significantly higher in group E, 2. There was no seasonal difference in mortality in group E, 3, In-hospital mortality in group E in 4 seasons did not differ significantly, 4, The cut-off value for food intake of 75% is optimal, 5. Multivariate analysis showed that the odds ratio of dietary intake as a predictive factor of in-hospital mortality was 0.616 (95% IC: 0.496 - 0.766, p < 0.001).
Conclusion: In-hospital mortality was significantly higher in group E and no seasonal difference exists. In-hospital food intake of three meals per day was a predictor of in-hospital mortality and its cut-off value was 75%.
Keywords: Emergency Admission; Nutritional Survey; Nutritionday; In-Hospital Mortality; Hospital Meal
Introduction
It is well known that inadequate food intake during or at the time of hospitalization or in the week before hospitalization correlates with worsening in-hospital mortality [1,2]. Since 2006, ESPEN has conducted a cross-sectional survey on an annual Thursday in November as the once-a-year instead of once-a-season nutritional survey (nutritionDay: nDay) among patients in Euroepan countries [3,4] and the others [5], staying in hospital or nursing home on that day [6-9] In this context, not only staying in intensive care unit (ICU) [10], staying general wards after from ICU [11], but emergency admissions are known to have a higher mortality rate than scheduled admissions, even on weekdays [12-14]. Due to the COVID-19 pandemic that started in 2019, the situation of emergency hospitalizations was greatly affected by COVID-19 for more than three years until the pandemic subsided [15,16]. However, as COVID-19 subsides, the situation returns to the same as before COVID-19, with emergency hospitalizations for cases other than COVID-19 infection. However, as noted above, it is not always easy to perform this assessment in emergency hospitalizations because of the priority of emergency treatment. In addition, it has been reported that food intake during one week prior to and on admission has been assessed and that mortality during hospitalization is high when the requirement is less than 50% [17]. Since it seems the priority to examine whether nutritional intake at any time after emergency admission is associated with mortality or not, to confirm whether it is or not, we conducted a cross-sectional observation of emergency department patients in four seasons to address the question of whether the effectiveness of once-a-year instead of once-a-season nutritional survey conducted in November is also observed in other seasons.
Objective
To test the validity of a once-a-day dietary survey rather than a once-a-seasonal survey, a cross-sectional dietary survey conducted once a year, to see if it is affected by seasonal variations.
Methods
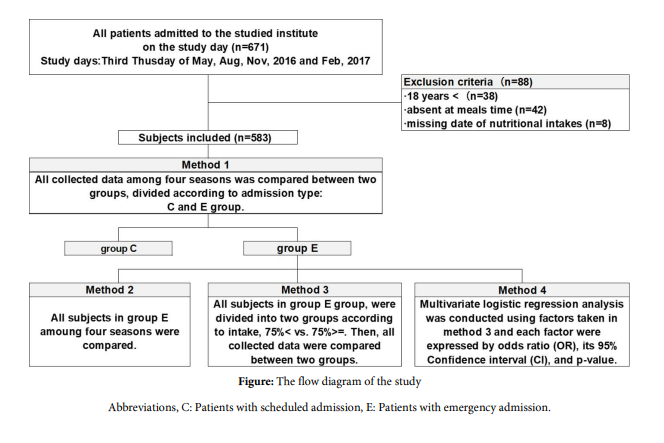
With reference to international annual surveys for nutritional assessment of inpatients and institutionalized people conducted once a year on the third Thursday of November, this study was conducted once a season with an occasional similar survey to test whether the validity of a once-a-day survey is sufficient and whether it is affected by seasonal effects. The study was conducted cross-sectionally in three consecutive months to cover four seasons, May followed by August, November and the following February. One of the reasons for choosing Thursday was to avoid weekend effects [6-9]. The enrolled subjects were all inpatients at the single hospital. Data were collected from electronic medical records and included; 1, Characteristics: age, sex, height (H), body weight (BW), body mass index (BMI, kg/m2) calculated by the equation of BW (kg) divided by H (m)2 , admitted word (Internal Medicine/ Surgery), Charlson comorbidity index (CCI) [18], activities of daily living (ADL), admission style of scheduled or emergency. Scheduled admissions were defined as admissions on the scheduled day and emergency admissions were the others. They were divided into two groups, control group (group C) and emergency group (group E), 2, nutritional parameters: an average dietary intake of 3 consecutive hospital foods on the day of the study for lunch, dinner and breakfast the next morning. Intake was categorized as four parts, more than 75%, 50%, 25% and less than 25% of the recorded amounts of each main and side dish separately. Food texture was also assessed using the International Dysphagia Diet Standardisation Initiative (IDDSI) score [19], 3, laboratory data: the highest C-reactive protein (CRP) and haemoglobin (Hb) during hospitalisation, the days between the date of the highest CRP measurement and the study date, expressed in number ± days from the study date, 4, Outcome measures: mortality during hospitalization as the primary outcome measure and length of stay (LOS), mortality within 30 days of admission and discharge to home as secondary outcomes, with the highest CRP during hospitalization. Exclusion criteria were: 1) age under 18 years, 2) who were not present at the ANU meal times, 3) missing food intake counts. We collected this information from the hospital electronic medical records of all subjects and examined the results using the following methods. The timeline of data collection is shown in Table 1. The data collected were analyzed using the following three methods.
Method 1: Comparison of outcome measures between group C and E
The data were compared between group C and E in each season separately to confirm the fact that outcome measures were worse in group E.
Once this was confirmed, all data in Group E across four seasons was combined and further analysis focused on Group E.
Method 2: Comparison of outcome measures in group E over four seasons
All data from Group E in each season were compared across the four seasons to determine whether or not there were seasonal differences in outcome measures in group E.
Method 3: Test for an effect of food size on outcome measures in group E
To test whether the amount of food consumed was associated with the outcome measures, all subjects in group E of four seasons were divided into two subgroups according to mean food intake >= vs < 75% or 50% of the amount of hospital food provided. In this method, the food intake thresholds were set at two different levels to ensure which was more predictive of outcomes in group E. They were set at 75% and 50% of the served amount in methods 3.
Method 4
A multivariate analysis as logistic regression analysis was performed to determine the predictive factors for the in-hospital mortality of patients in group E.
Ethic Statement
The ethical considerations were approved by the Ethic Committee of the studied hospital and the approval number is 2017-200. In order to obtain ethics committee approval, an opt-out procedure was published in the hospital and on the website, stating that patients admitted during the study period who did not wish to participate should inform the hospital of their wishes.
Statistical Analysis
Data are presented as median, 25th percentile, and 75th percentile. The Mann-Whitney U test was used for differences in median values between two groups, the KruskalWallis test for comparisons between four groups, and the χ2 test or Fisher's exact test for differences in proportions between groups. Multivariate logistic regression analysis with adjusted odds ratio's for in-hospital mortality was performed. The adjusted odds ratios, 95% confidence intervals and their P-values represent the odds of in-hospital mortality after adjusting for the covariates listed in the table. A statistically significant difference was considered significant when p < 0.05. Statistical analysis was performed with SPSS version 29 (IBM, Armonk, NY, USA).
Results
The total number of hospitalized patients on the four study days of the four seasons on the seasonal nDay was 671. After excluding 88 patients due to exclusion criteria, the remaining 583 patients were included in the study.
Result 1
Compared to group C, group E was older, had a lower BMI and body weight, and had a higher CCI, which indicates the number of minor comorbidities, all of which were statistically significant. In addition, food intake < 75% of requirements of the study days, food texture scored by IDDSI, and in-hospital mortality as the primary outcome, the length of stay (LOS), the highest CRP during the entire hospital stay, the in-hospital death rate within 30 days, and discharge to home were significantly worse in group E (Table 2).
Result 2
All descriptions of patients with emergency admission in four seasons were not significantly different (Table 3). Similarly, comparing emergency hospitalization patients in four seasons in group E, food intake < 75% of requirements of the study days, food texture scored by IDDSI, ADL score < 3, and in-hospital mortality as the primary outcome, the length of stay (LOS), the highest CRP during the entire hospital stay, the date of measurement of the highest CRP value, converted from the date of the study, the death rate during hospitalization within 30 days, were not significantly different.
Since there were no differences in the mortality rate of patients involved in group E among four different seasons, all data of group E were gathered in further analyses
Result 3
Food intake, food texture scored by IDDSIS, and In-hospital mortality as the primary outcome measure, as well as length of stay (LOS), highest CRP during the entire hospital stay, and in-hospital mortality within 30 days were significantly worse in patients who consumed less than 75% of the in-hospital food compared to those who consumed >= 75% (Table 4, left column shaded area).
When these results were obtained, we further performed a similar analysis of all emergency hospitalized patients using the conventional nDay cut-off of 50% (Method 4). The results showed that the in-hospital mortality rate was higher in the group with less than 50% admission, as was the case when the cut-off was set at 75% (Table 4, right column blank area).
Result 4
As the predictors of in-hospital mortality in patients admitted emergency type were examined by logistic regression analysis, it was the result that the odds ratio (OR) for in-hospital mortality compared to average food intake was 0.616 (95% IC: 0.496 - 0.766, p < 0.001), indicating that intake was a predictor of in-hospital mortality in emergency patients (Table 5).
Discussion
Why do emergency admissions have a higher mortality rate than scheduled admissions?
The in-hospital mortality rate was higher for emergency admissions than for scheduled admissions, and the length of stay was significantly longer (27 days vs. 20 days, p < 0.001).
Predictive indicators were reported for each country, using length of hospital stay as the outcome indicator [20]. Other studies have also confirmed the high in-hospital mortality rate for emergency admissions [12-14]. Moreover, the most important variable in prediction was the number of emergency department (ED) visits in the previous year [17]. Reasons for in-hospital mortality in ED include the lack of hospital staff during off-hours and the time required for treatment tools and surgical procedures. However, in this study, CRP was also significantly higher in emergency patients (6.7 vs. 1.7 mg/dL, p < 0.001).
Mortality of patients in group E do not differ by seasonality
Accident and emergency (A&E) attendances in England and other countries have increased by more than 35% in the last 10 years [18]. This high and increasing demand for emergency care is putting severe pressure on A&E departments, and long waiting times and poor quality of care are a cause for concern. Many explanations have been put forward for the increasing trend, including population growth and aging, overstretched social and elderly care systems, poor access to primary care, lack of family support, and increased patient awareness of symptoms of acute conditions. There is evidence from the US that there are strong seasonal variations in the demand for health care by people, usually of retirement age, who migrate to states with milder climates during the winter months. In contrast, there is no tendency for the elderly to migrate in the year of the study to avoid the cold winter. In other words, as can be seen from the results, there is no seasonal difference in the age of group E. Furthermore, there were no differences in subjects' descriptions and nutritional status, such as BMI, CCI, ADL, and food intake, and there were no seasonal differences in in-hospital mortality, length of stay, or in-hospital CRP (Table 2). This result confirms the validity of the fact that nDay surveyed in November can be applied to other seasons
75% of dietary intake rather than 50% as an earlier predictor of adverse events in group E
The food intake categories included in the MST, GLIM criteria, nDay questionnaire [21], or a mixed type with other indicators including food intake variables [22] were used for nutritional screening of hospitalized patients are all 100%, 50%, 25%, and 0%. In contrast, only NRS2002 has one of the food intake cutoffs set at 75% of the requirement. Another reason for choosing 75% as a candidate cutoff is that ward nurses who count food intake can relatively easily determine if less than 75%of the food is left on the plate by just looking at it.
Since there was no seasonal difference in the mortality rate in the E group, we decided to combine the four seasonal subjects into the E group. There was a significantly higher mortality rate in the group with less than 75% of intakes. An intake as a cut-off value for predicting survival was 50%, and 75%, which is predicted to appear earlier than the 50% newly introduced in this study, was the first known predictor of alcohol rice field. Next, we tested whether the cutoff for food intake for emergency hospitalized patients, the traditional 50% or the newly introduced 75%, seems more useful. In addition, it is relatively easy to visually determine whether 75% of the dose has been taken, and it does not place a large workload on nurses on the ward, making it possible to identify patients with poor outcomes early and improve outcomes. This is expected to be a powerful method. However, the differences of outcome measures were not different, it still not significant that 75% as cutoff is more helpful than 50% to draw emergency patients with higher mortality. For the above reasons, we added the multivariate analysis whether continuous variable of food intake is associated with mortality or not.
Strengths and Limitations of the present study
Strengths of this study include the following two points: 1, no seasonal effect on higher in-hospital mortality among emergency hospitalized patients compared with scheduled hospitalized patients; 2, we clarified that a given daily food intake is a predictor of high mortality for the first time.
On the other hand, the following limitations of this research should be mentioned. First, due to the small number of subjects and the fact that these are retrospective and non-randomized studies, it is necessary to consider the existence of subject and method bias. Second, although the nDay survey was conducted on Thursdays, it will be necessary to test whether the malnutrition survey is valid on other days of the week and whether there is day-of-week specificity. Third, by setting the cutoff for food intake, it is still to be resolved which is a predictor of mortality in emergency room patients, at 75% instead of the traditional 50% for early prediction of in-hospital mortality. The lack of analysis of not only intake but also energy, protein, and micronutrient intakes is another limitation of this study [23]. Fourth, although a 75% cutoff for intake was obtained in this study, cutoffs for nutrient content such as energy, protein, macronutrients, and micronutrients were not verified. I look forward to seeing the results of future research.
Fifth, the inverse relationship between inadequate hospital food intake and mortality has been speculated due to the lack of macro- and micronutrients as anti-inflammatory substances. However, this was not scientifically proven in this study and needs to be validated.
Conclusion
In-hospital mortality was significantly higher in group E and no seasonal difference exists. In-hospital food intake of three meals per day was a predictor of in-hospital mortality and its cut-off value was 75%.
Source(s) of Financial Support in the form of Grants
None
Statements and Declarations Regarding Conflicts of Interest
All authors have no conflicts of interest to disclose
Author Contribution
Authors made the following contribution to the manuscript: HM, AT, TA formulated the original idea, HM completed the database search, data extraction and analysis, HM, TA drafted the manuscript, YH, EY reviewed and revised the manuscript for important intellectual content, and all authors provided final approval of the version to be submitted.
- Hiesmayr M, Schinder K, Pernicka E, Schuh C, Schoeniger-Hekele A, Bauer P, et al. (2006) NutrtionDay Audit Team. Decreased food intake is as risk factor for mortality in hospitalized patients: the Nutriton Day survey 2006. Clin Nutr, 28: 484-91.
- Tsaousi G, Panidis S, Stavrou G, Tsouskas J, Panagiotou D, Kotzampassi K (2014) Prognostic indices of poor nutritional status and their impact on prolonged hospital stay in a Greek university hospital. Biomed Res Int. 2014: 924270.
- Ostrowska J, Sulz I, Tarantino S, Hiesmayr M, Szostak-Węgierek D (2021) Hospital Malnutrition, Nutritional Risk Factors, and Elements of Nutritional Care in Europe: Comparison of Polish Results with All European Countries Participating in the nDay Survey. Nutrients. 13: 263.
- Ostrowska J, Sulz I, Tarantino S, Hiesmayr M, Szostak-Węgierek D (2021) Hospital Malnutrition, Nutritional Risk Factors, and Elements of Nutritional Care in Europe: Comparison of Polish Results with All European Countries Participating in the nDay Survey. Nutrients. 13: 263.
- Zhou B, Zhang Y, Hiesmayr M, Gao X, Huang Y, Liu S, et al, (2024) On Behalf Of The nutritionDay Chinese Working Group. Dietary Provision, GLIM-Defined Malnutrition and Their Association with Clinical Outcome: Results from the First Decade of nutrition Day in China. Nutrients. 16: 569.
- Cardenas D, Bermúdez C, Pérez A, Diaz G, Cortés LY, Contreras CP, et al. (2022) Are traditional screening tools adequate for monitoring the nutrition risk of in-hospital patients? An analysis of the nutrition Day database. JPEN J Parenter Enteral Nutr. 46: 83-92.
- Torbahn G, Sulz I, Großhauser F, Hiesmayr MJ, Kiesswetter E, Schindler K, et al. (2022) Predictors of incident malnutrition-a nutrition Day analysis in 11,923 nursing home residents. Eur J Clin Nutr. 76: 382-8.
- Schindler K, Pichard C, Sulz I, Volkert D, Streicher M, Singer P, et al. (2017) nutrition Day: 10 years of growth. Clin Nutr. 36: 1207-14.
- Graeb F, Wolke R (2021) Malnutrition and Inadequate Eating Behaviour during Hospital Stay in Geriatrics-An Explorative Analyses of Nutrition Day Data in Two Hospitals. Nurs Rep. 11: 929-41.
- M Miguélez, C Velasco, M Camblor, J Cedeño, C Serrano, I Bretón, et al. (2022) Nutritional management and clinical outcome of critically ill patients with COVID-19: A retrospective study in a tertiary hospital. Clin Nutr. 41: 2940-6.
- Fischer A, Veraar C, Worf I, Tarantino S, Kiss N, Schuh C, et al. (2023) More Nutritional Support on the Wards after a Previous Intensive Care Unit Stay: A nutrition Day Analysis in 136,667 Patients. Nutrients. 15: 3545.
- Ricciardi R, Roberts RL, Read TE, Baxter NN, Marcello PW, Scholetz DJ (2011) Mortality after non-elective hospital admission. Arch Surg. 146: 545-51.
- Walicka M, Tuszyńska A, Chlebus M, Sanchak Y, Śliwczyński A, Brzozowska M, et al. (2021) Predictors of in-hospital mortality in surgical wards: a multivariable retrospective cohort analysis of 2,800,069 hospitalizations. World J Surg. 45: 480-7.
- Chen L, Chen L, Zheng H, Wu S, Wang S (2021) Emergency admission parameters for predicting in-hospital mortality in patients with acute exacerbation of chronic obstructive pulmonary disease with hypercapnic respiratory failure. BMC Pulm Med. 21: 258.
- Fatema Calcuttawala.. Nutrition as a key to boost immunity against COVID-19. Clin Nutr ESPEN. 49: 17-23.
- Shankar K, Chandrasekaran R, Venkata PJ, Miketinas D (2023) Investigating the Role of Nutrition in Enhancing Immunity During the COVID-19 Pandemic: Twitter Text-Mining Analysis. J Med Internet Res. 25: e47328.
- Chiu YM, Courteau J, Dufour J, Vanasse A, Hudon C (2023) Machine learning to improve frequency emergency department use predictor: a retrospective cohort study. Sci Reports. 13: 1981.
- Forchini G, Hauck K, Steventon A (2024) Seasonal and regional fluctuations in the demand for Accident and Emergency care in English hospitals.970, Umeå University, Department of Economics.
- IDDSI (2023) Complete IDDSI framework detailed definitions 2.0/2019.
- Kiss N, Hiesmayr M, Sulz I, Bauer P, Heinze G, Mouhieddine M, et al. (2021) Predicting Hospital Length of Stay at Admission Using Global and Country-Specific Competing Risk Analysis of Structural, Patient, and Nutrition-Related Data from nutrition Day 2007-2015. Nutrients. 13: 4111.
- Schindler K, Themessl-Huber M, Hiesmayr M, Kosak S, Lainscak M, Loviano A, et al. (2016) To eat or not to eat? Indicators for reduced food intake in 91,245 patients hospitalized on nutritonDays 2006-2014 in 56 countries worldwide: a descriptive analysis. Am J Clin Nutr. 104: 1393-402.
- Jeejeebhoy KN, Keller H, Gramlich L, Allard JP, Laporte M, Duerksen DR, et al. (2015) Nutritional assessment: comparison of clinical assessment and objective variables for the prediction of length of hospital stay and readmission. Am J Clin Nutr. 101: 956-65.
- Sanchez M, Courtois-Amiot P, Capdepon A, Neveux N, Gautry J, Dorigny B, et al. (2023) Four-week administration of an energy and protein dense oral nutritional supplement improves micronutrient concentrations but does not completely correct deficiencies in institutionalized malnourished older adults. Front Nutr. 10: 1249936.

Tables at a glance
Figures at a glance