Covid-19 Psychomental and Socio-Behavioural Effects on Patients and Health Professionals at Laquintinie Referral Hospital, Douala, Cameroon
Received Date: October 10, 2023 Accepted Date: November 10, 2023 Published Date: November 13, 2023
doi: 10.17303/jnnd.2023.11.104
Citation: Ernest Tambo, Nadine Nague, Serge Bruno Ebong, Ngo T. Tappa, Bertin Fankep, Jules Assob (2023) Covid-19 Psy chomental and Socio-Behavioural Effects on Patients and Health Professionals at Laquintinie Referral Hospital, Douala, Cameroon. J Neurophysiol Neurol Disord 11: 1-15
Abstract
COVID-19 pandemic remains a major public health and global health problem. It continues to have significant effects at different levels, and poses a significant threat to mental health. A cross-sectional analytical study on the influence of COVID-19 on the psycho-mental health of health professionals and patients was carried out at Laquintinie Hospital in Douala during a period of 08 months from January 2021 to August 2021. Using the modified and pre-tested form of the Hospital Anxiety and Depression Scale (HADS), we collected data according to the WHO guide to psycho-mental health. A questionnaire was implemented to assess the contribution of anxiety and depressive symptoms. After informed consent, a group of 500 people was interviewed, including 158 health workers and 342 patients. The results show a high rate of anxiety, depression and stress (17.3%; 29.63% and 47.57%) respectively among health workers and a rate of anxiety, depression and stress (7.84%; 9.85% and 15.74%) respectively in patients. There is a high susceptibility to depression in subjects aged 51 years and over [OR (95% CI) 2.16 (1.18-3.96), P = 0.012], and a high susceptibility to anxiety over the department of medicine [OR (95% CI) 3.73 (1.40-9.92) P = 0.005]; Have been associated risk factors in patients. On the other hand, among health professional, males were more likely to be stressed [OR (95% CI) 2.04 (1.81-4.71), P = 0.022], married men [OR (95% CI) %) 1.46 (1.31-1.62) P = 0.034] and the department of medicine [OR (95% CI) 5.73 (1.29-24.4) P = 0.011] had a higher risk of have depression; in addition, the emergency-anesthesia and resuscitation department were at greater risk for anxiety. In addition, correlation analyses showed a statistically significant link between professional and anxiety, lack of water, disinfectant points and suicide in health structures, respectively (P = 0.036 ; P = 0.010).There was a statistically significant relationship between depression and lack of social and mental support programs from those around him (P = 0.05); stress and the onset of COVID-19 in Cameroon, (P = 0.000). The establishment of a system of advice, assistance and / or specialized psycho-mental health support in all district hospitals in Douala and its surroundings in the context of current and post pandemic.
Keywords: COVID-19; Depression; Anxiety; Mental Health; HADS; Health Professionals; Patients; Cameroon
Introduction
COVID-19 pandemic exposed local, regional and global health system vulnerabilities and weaknesses. The mental health neglected has had a profound socioeconomic and health impact in several ways. COVID-19 has shown, more than ever, to what extent mental health is an integral part of health and well-being and must be an essential part of health services during health emergencies [1].The death rate and the risk of contagion have turned out to be much higher than expected. The caregivers faced a poorly understood and fatal disease, and also were very distressed to contract this disease and pass it on to their loved ones [2].The health and economic consequences of the epidemic are glaring, but this crisis is also having psychological repercussions on the affected populations. More difficult to demonstrate, but no less important, these consequences on the psycho-- mental and socio-behavioural health of populations are of increasing concern to professionals. Despite the fact that COVID-19 is one of the first coronavirus infections to be the subject of mental health studies, it was quickly brought under control, and had significant health, psychological and social consequences [3]. Chua et al., showed that the immediate psychological sequelae of COVID-19 involved a significantly higher stress level in affected individuals, when compared to match healthy controls [4].Lee et al., Have reported the presence of episodes of acute psychosis in a few SARS patients [5].
Recent studies on COVID-19 show that it is more deadly and more invasive than SARS of 2002, both healthy and psychologically. This underlines its significant impact on psychological health. In a study, Lai and his colleagues assessed the effects of SARS on the mental health of healthcare professionals in China in 2003. The results reveal a considerable proportion of participants who reported symptoms of depression (50.4%), anxiety (44.6%) and distress (71.5%).These data suggest that healthcare workers, on the front line of the response to the disease, are severely strained psychologically and may develop significant psychological distress, which is the source of a potentially disabling anxious experience [6].Although there is little data on how the new coronavirus is worsening mental health problems on the African continent. A survey of 12,000 women in low-income communities in Uganda and Zambia found increased persistent stress, anxiety and depression, as well long term psychmental and behavioural effects on professional, survivors and populations [7].
However, in the agenda of human development in Africa, less than 10% of the population has access to mental health care. A problem amplified by the lack of mental specialists and social protection support coupled with limited qualified human resource. It has been noted that, the majority of African countries have one psychiatrist per 500,000 inhabitants, instead of one psychiatrist per 5,000 people in accordance with WHO recommendations [8].
The Hospital Anxiety and Depression Scale (HADS) can be used as a powerful tool to assess anxiety and depressive symptoms using a pre-structured and tested questionnaire sent to professional groups in the 10 regions of the country, prior to their informed consent. A recent study conducted on 331 healthcare professionals interviewed in 2020 showed a 41.8% anxiety and 42.8% depression. There was a higher susceptibility to depression in young subjects (30-39 years). Fear of contamination and fear of death are modulators of depression and anxiety. The anxiety-depression comorbidity in the sample is 14.73%. The prevalence rates of major depressive disorder and adjustment disorder in the sample are 8.2% and 3.3%, respectively in Cameroon [9]. Yet, little is documented on the psychomental and socio-behavioural states and COVID19 pandemic effects on Health workers and patients in Cameroon.
The study was to determine COVID-19 psychomental and socio-behavioural effects on healthcare professionals and patients attending the Laquintinie Hospital in Douala, Cameroon.
Methods
Study Design, Setting and Population
A cross-sectional and analytical study with a prospective aim was conducted at the Laquintinie hospital in Douala from January to August 2021. Our study population consisted of healthcare professionals and patients attending Laquintinie Hospital in Douala who had consented to participate in our study
Sampling Technique
A non-probability and convenience sampling technique was used for questionnaire administration. This method can be justified based on the mere fact that all health staff and patients attending hospital for care and service delivery during COVID were randomly selected with distinction of and if consented, the research study was verbally explained to each and upon common consensus the questionnaire was administered. The sample size was defined by the Lorentz formula, so a minimum size was 500 Participants.
Data Collection Tools, Procedure and Quality Control
We used a Questionnaire and the modified and pre-tested Hospital Anxiety and Depression Scale (HADS) in accordance with the WHO guide (it comprises 14 items and rated from 0 to 3. From 0-7 normal, from 8-10 moderate, from 11 -14 medium and 15-21 severe [10]. The questions in Even numbers were that of Anxiety and in Odd numbers were that of Depression for this part which is found in the appendix), For the nursing staff and patients attending the various departments of the HLD.
The data collected has been reviewed and verified for consistency and clarity; completeness, and accuracy throughout the data collection process. We distributed this questionnaire to all participants who consented to participate in the survey after a comprehensive dialogue and communication prior administration.
Data Analysis and Statistical Tools
An input mask was mounted on Excel and the data was entered in the same software, then analyzed on SPSS version 23.0. Chi-square and logistic regression tests were performed. We carried out the varied, bi-varied and multivariate analyzes to produce our results. The corresponding confidence interval is 95%. The significance level was at p < 0.05.
Ethics Statement
Ethical authorization was obtained from the institutional research ethics committee for human health at the University of Douala and administrative authorization from the director of the Laquintinie hospital in Douala. Written and verbal consent was obtained from each study participant prior to the data collection process. During the data collection process, we informed each study participant about the expected benefits of the research project.
Results
1-Sociodemographic Characteristics of the Study Population
Our study involved a sample of 500 participants including 158 healthcare workers and 342 patients attending the Laquintinie Hospital in Douala. The distribution of the results by sex shows that the female sex was more represented 51.17% than the male sex 43.83% in the patients. The distribution by age groups shows that it is the [18-30 years] who are the most represented of the samples 32.16% in the patients and that of [31-40 years] of 44.94% in the personal health. This study reveals that 38.60% of the respondents were traders; 34.21% of housewives; 14.91% of government; and 12.28% of students for patients (Table I).
On the other hand, among the health professional, nurses represented the majority of 28.75%; 17.09% of physicians; 15.19% of surface technicians and 10.13% of laboratory technicians. The most represented services in the sample were that of the care and services department 82.69% among patients and 100% of the hygiene and sanitation department among health professional (Table 1).
2- Evaluation of the Socio-Cultural and Anthropological Perceptions of the Respondents
This study shows that 96.2% of healthcare worker respondents said that COVID-19 could cause stress, anxiety and depression in an individual and 3.8% who said it could not cause. Our findings show that 33.1% of patients took traditional potions and 89.2% of health professional respected the barrier measures. P = 0.001. 29.6% of patients and 31.2% of health workers said that my family is afraid of touching me for fear of being infected. P = 0.038. Accordingly, 12.2% of Patients said they were afraid they would be injected with the COVID-19 vaccine since being hospitalized in this department. As well, 24.3% of health workers responded that they are afraid that all health workers will be forced to take this vaccine or make the vaccination mandatory (P = 0.001) (Table 2).
We also reported that a statistically significant relation between I think this could reduce the number of cases of people infected with Covid and COVID-19 vaccination (P=0.0019)
3- Treatment of COVID Patients with Psycho-mental Disorders
Only 14.9% of respondents from the medical department said they administered the COVID Protocol and psychiatric follow-up. P = 0.001. COVID Protocol + Psychiatric follow-up was strictly adherence and respect to biosafety guidelines, standard clinical and laboratories operating procedures including environmental protective measures by all staff and COVID-19 patients and visitors in all departments in referral hospital ) (P=0.00). Whereas the referral isolation and followed by psychiatry was not statistically significant in all those units (Table 3).
3- Factors Associated with Anxiety and Depression Rates Among Healthcare Professional and Patients Attending HLD
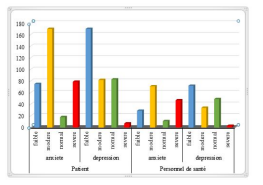
Our results show us that at the level of COVID-19 severity of respondents on the HADS scale, that when one considers the degree of severity of anxiety and depressive symptoms, we observe a higher prevalence of moderate symptoms on the HADS scale. anxiety with 50% and low 50% on depression in patients; then sever00e symptoms on anxiety 30% and moderate on depression with 22% among health workers(Figure 1).
5. Rate of Anxiety, Depression and Stress in HLD Patients
The age at 51 years and over, ie 22.2% of respondents (95% CI) 2.16 (1.18-3.96), P = 0.012]; the Department of Medicine or 44% of respondents [OR (95% CI) 3.73 (1.40-9.92) P = 0.005] were factors associated with the risk of depression and anxiety, respectively. Furthermore, respondents presented COVID-19 work related anxiety rate of 7.84%; depression at 9.85% and COVID-19 work related stress at 15.74% (Table 4).
The male sex, i.e 34.7% of the respondents [OR (95% CI) 2.04 (1.81-4.71), P = 0.022] were a factor associated with the risk of stressing; the married or 41.3% [OR (95% CI) 1.46 (1.31-1.62) P = 0.034]; the department of medicine or 9.2% [OR (95% CI) 5.73 (1.29-24.4) P = 0.011] were factors associated with the risk of developing depression; the department of emergencies-anesthesia and reanimation or 38.8% [OR (95% CI) 18 (3.12-103.74) P = 0.000] were a factor associated with the risk of developing anxiety. In addition, our respondents have an anxiety rate of 17.3%; depression at 29.63% and stress at 47.57% (Table 5).
4- Correlations Between Factors and Impact of Covid-19 on Psycho-Mental Health
Our results in patients organizational factors that may influence COVID19 on mental and socio-behavioural health showed that 60% of respondents who spoke of Personal protective equipment deficiency were stressed P = 0.004; 58.6% who spoke of the disruption of daily lifestyle of family and social activities were anxious P = 0.010. On COVID-19 work stress risk factors, 67.5% of respondents who spoke about fear of death were stressed, P = 0.003. As for the feeling since the COVID-19 pandemic confinement and lockdown measures showed that 97.7% of respondents said they were depressed in Cameroon (P = 0.002) (Table 6).
Among health professional, On Organizational Factors That May Influence Covid19 on mental Health. Our results showed that 51% of respondents who spoke about Lack of water points and disinfectant in businesses / health facilities were Anxious P = 0.036. For stress risk factors 20.2% of respondents who spoke of the lack of support from those around them were depressed P = 0.05. Speaking of the consequences of COVID-19 in society 2.7% of our respondents who spoke about suicide were anxious P = 0.010 (Table 7).
Discussion
The study reported an increasing prevalence of moderate symptoms on anxiety with 50% and low 50% on depression in patients, then severe symptoms on anxiety 30% and moderate on depression with 22% among healthcare workers. These results are contrary to that of a study by S. Li, Wang, et al which found a strong presence of symptoms of anxiety 41.8% and depression 42.8%, and found a degree severity 26.5% for anxiety and 33.1% for depression) [11]. This shows that healthcare workers experienced more anxiety, depression and stress unlike patients who were more stressed at the time of our study. The patients were stressed by the fear of dying, anxious by the upheaval of daily life, family and social. On the other hand, the health professional were anxious by the lack of water points and disinfectant in the health structures; depressed by the lack of support from those around them; stressed by the outbreak of COVID-19 in Cameroon.
The stress of COVID-19 pandemic and the response measures exacerbated the already high psychological suffering of health workers. The health system and the organization of healthcare have found themselves more disrupted among nurses in particular as the general population continues to be psychologically affected by this major health crisis disruption, supply chain rupture of protective equipment and lack of COVID-19 and palliative products. This suggests that COVID-19 continues to affect the mental and socio-behavioral health of patients and healthcare workers. Among these problems, COVID-19 and safety work stress was the most expressed manifestation 47.57%, followed by depression 29.63%, then anxiety 17.3% among health workers and 15.74% for stress, followed by of depression 9.85% and finally 7.84% for anxiety. Huang and Zhao estimated the overall prevalence of GAD (Generalized Anxiety Disorder) at 35.1%; that of depression 20.1% [12].
Age over 51 years old was a risk factor for depression, this is consistent with Lu et al., elderly people state of immunosuppression, is likely to develop depression [13]. Male sex was a risk factor for stress as Eléonore SOLE reported on the psychological effects of confinement in a meta-analysis that pointed out symptoms of post-traumatic stress, depression, anger, fear, drug abuse, but especially morale at half-mast in humans [14]. Leveraging on digital technology in improving early risk communication and community engagement is crucial, while promoting collaborative and inclusive working mental and socio-behavioural systems and equity in the emergency-intensive care and resuscitation department is crucial a risk factor for anxiety [15,16].
This underlines the need to take into account the effects of COVID-19 on the mental health of health professional and patients of the Laquintinie Hospital in Douala-- Cameroon; which should result in the establishment of a psychological assistance and social protection support system [15,16]. We noted few limitations, as the study was conducted in only one referral hospital and no COVID-19 treatment center was considered. The modified WHO questionnaire could varied based on sociocultural and other factors where the mental health response programs is weak across Cameroon. Our findings could not be generalizable and benefits linked to facility-response improvements.
Conclusion
COVID-19 pandemic remains a major local and global health problem. It continues to have significant effects at different levels, and poses a significant threat to mental health. Our study reported that COVID-19 and work related anxiety, depression and stress rates were 17.3%, 29.63% and 47.57% among health professionals compared to anxiety, depression and stress rates of 7.84%, 9.85% and 15.74% in patients respectively. This requires taking into account the COVID 19 emergency confinement and lockdown response interventions and measures have had significant mental and behavioural health effects on health professional and patients. We call on government and stakeholders to advocate and promote investment, ample and sustained financial allocation in the establishment facility- and community-based psychological and socio-behavioural change support system and social protection or insurance emergency policies and programs deployment, sufficient resources to curb the unprecedented immediate and longterm psychomental and health consequences.
Ethical Approval and Consent to Participle
All participants consented and approved prior engagement into the study
Consent for Publication
All authors read and approved the final version for publication
Data Availability
Additional data can be made available upon request.
Competing of Interest
Authors have no conflict interests.
Funding
No funding support was received
Author’s Contributions
ET conceived the research topic. ET and NN modified, tested and adopted the contextual HADS protocol. NN conducted the field study and analyzed the data. ET and NN design the analytical plan and ET drafted of the manuscript. NN, BF, NTT, DT, ET and CJA improved the manuscript. All authors read and approved the final version.
Acknowledgement
We are thankful to Africa Disease Intelligence, Preparedness and Response (ADIPR) management for the enabling research environment and support.
- W Guan, Z Ni, Yu Hu, W Liang, C Ou, J He et al. (2020) Clinical characteristics of coronavirus disease 2019 in China N Engl J Med 332: 1708-20.
- SKW Cheng, CW Wong, J Tsang et al. (2004) Psychological distress and negative appraisals in survivors of severe acute respiratory syndrome (SARS) Psychol Med 34: 1187-95.
- United Nations, Briefing Note: COVID-19 and the Need for Action on Mental Health, May 2020.
- 4. Charlson, van Ommeren, Flaxman, Cornett, Whiteford, Saxena (2019) New WHO prevalence estimates of mental disorders in conflict settings: with systematic review and meta-analysis.
- WHO (2020) Impact of COVID-19 on mental health, neurological and addiction services.
- DTS Lee, YK Wing, HCM Leung et al. (2004) Factors associated with psychosis among patients with severe acute respiratory syndrome: a case-control study Clin Infect Dis 39: 1247-9.
- Chung RY, Dong D, Li MM (2020) Socioeconomic gradient in health and the covid-19 outbreak. BMJ 369: m1329.
- Alima covid19 in Cameroon: the challenges of integrating mental health in the response to the pandemic 08/10/2020
- Huang C, Wang Y, Li X et al. (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet.
- WHO P Barczack, N Kane, S Andrews, AM Congdon, JC Clay, T. Betts (1988) Patterns of psychiatric morbidity in a genito-urinary clinic: a validation of the Hospital Anxiety Depression scale (HAD) Brit J Psychiat 152: 698-700.
- S Li Wang, Cheng, CW Wong, J Tsang et al. (2004) Psychological distress and negative appraisals in survivors of severe acute respiratory syndrome (SARS) Psychol Med 34: 1187-95.
- Y Huang, N Zhao (2020) Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 epidemic in China: a web-based cross-sectional survey.
- Lai J, Ma S, Wang Y (2020) Factors associated with mental health outcomes among health care workers exposed to Coronavirus disease 2019. JAMA Netw Open 3: e203976.
- Eléonore SOLE Futura health. Containment: what psychological effects on humans?
- Ernest Tambo, Ingrid C Djuikoue, Gildas K Tazemda, Michael F Fotsing, Xiao-Nong Zhou (2019) Early stage risk communication and community engagement (RCCE) strategies and measures against the coronavirus disease 2019 (COVID-19) pandemic crisis,Global Health Journal 5: 44-50.
- Lal A, Ashworth HC, Dada S, Hoemeke L, Tambo E (2022) Optimizing Pandemic Preparedness and Response Through Health Information Systems: Lessons Learned From Ebola to COVID-19. Disaster Med Public Health Prep 16: 333-40.

Tables at a glance
Figures at a glance