Corneal Remodeling of Laser Asymmetric Keratectomy Combined with Collagen Cross Linking in Patients with Keratoconus Suspect
Received Date: September 06, 2023 Accepted Date: October 06, 2023 Published Date: October 09, 2023
doi: 10.17303/jooa.2023.7.102
Citation: Byung Moo Min (2023) Corneal Remodeling of Laser Asymmetric Keratectomy Combined with Collagen Cross Link ing in Patients with Keratoconus Suspect. J Ophthalmol Open Access 7: 1-10
Abstract
Objectives: To evaluate a new corneal remodeling technique of LASEK with laser asymmetric keratectomy combined collagen cross linking (L-LAK-CXL) in myopic patients with keratoconus suspect (KCS)
Methods: 23–40-year-old four myopic (-1.75 - -4.75 D) patients (4 eyes), of KCS with focal corneal steepening over +47.0 D and peripheral asymmetric corneal thickness were included in this study. L-LAK-CXL was performed both original ablation of refractive errors and customization ablation of thicker peripheral cornea (50-76 µm) selectively and myopic change (-1.25 – -1.75D) due to the ablation of eripheral thicker cornea simultaneously under intergration of Vision Up software, and then performed CXL without epithelium. We measured pre-and postoperative ocular findings including the sum of corneal thickness deviations in four directions (SUM), decenteration of the thinnest point (DISTANCE), and TBUT.
Results: SE (D, average) decreased fr om -3.44 preoperatively to -0.34 postoperatively. UDVA (LogMAR, average) increased from 0.93 preoperatively to 0.00 at postoperative and Kmax (average, D) had decreased from +48.00 preoperatively to +43.88 at postoperative, IOP and pupil size were similar between pre- and postoperative. Central pachymetry (µm, average) decreased from 581 to 508. Postoperative corneal symmetry increased markedly due to decreased SUM and DISTANCE (from 165 to 63µm, from 1.02 to 0.28, respectively). TBUT (seconds) increased from 5.78 preoperatively to 18.56 postoperatively. There was no postoperative corneal ectasia.
Conclusion: L-LAK- CXL improved corneal symmetry in four myopic patients with KCS by reducing the SUM, DISTANCE, increasing TBUT and showing good postoperative visual outcomes.
Keywords: Keratoconus Suspect; Focal Steepening; Regional Asymmetry of Corneal Thickness; Corneal Symmetry; New Corneal Remodeling
Introduction
Keratoconus (KC) is a well-defined progressive corneal ectasia characterized by steepening corneal curvature, changes in refractive error and changes in corneal thickness that result in visual impairment [1].
Definition of keratoconus suspect (KCS) is not defined, and there are several opinions for definition [1-9]. KCS has been showed focal steepening maybe over +47.0 D, an asymmetrical, truncated or skewed-axis bowtie [2], central corneal thickness less than 500um, oblique astigmatism more than 1.5D [3] but did not result in visual impairment. On diagnosis of KCS, Scheimpflug corneal topography and epithelial mapping by corneal OCT were currently used [10,11].
True KCS are an absolute contraindication to LASIK or photorefractive keratectomy due to postoperative ectasia [12].
Of these findings of KCS, focal steepening over +47.0 D and peripheral corneal asymmetry of the thickness could be very important because of the possibility of postLASIK or PRK corneal ectasia. In myopic patients with topographic asymmetry of the corneal thickness and steep corneal curvature more than +47.0D, LASIK or PRK only cannot avoid postoperative corneal ectatic changes, possibly the postoperative thinner regions of the cornea are more likely to be steepened as a result of corneal biomechanical interaction of corneal thickness, corneal stiffness and intraocular pressure, leading to increased changes in optical aberrations [13,14]. The introduction of eccentric thinning was required to produce asymmetric displacement and an eccentric peak in dioptric curvature value if a normal elastic modulus was use [14]. Recently laser asymmetric keratectomy (LAK) as customization method, integrated with Vision Up software (Well C, Busan, South Korea) has yielded good results and the maintenance of corneal symmetry in myopic patients with peripheral asymmetric cornea of the thickness because it could ablate only thicker peripheral cornea selectively as customization method [15-20].
In collagen cross linking, riboflavin (vitamin B2) is administered in conjunction with ultraviolet A (UVA, 365nm). The interaction of riboflavin and UVA cause formation of reactive oxygen species, leading to the formation of additional covalent bonds between collagen molecules, with consequent biomechanical stiffing of the cornea [21-23].
The present study showed the initial result of a new corneal remodeling technique of L-LAK-CXL to correct refractive errors (original ablation) and peripheral corneal asymmetry of the thickness (customization ablation) simultaneously, in myopic patient with KCS, accompanied by peripheral asymmetry of corneal thickness (a SUM of ≥80 µm) and focal corneal steepening (Kmax) over + 47.0 diopters.
Methods
This retrospective study included patients who were treated at the Woori Eye Clinic between February 2019 and October 2020. This study was conducted in accordance with the Declaration of Helsinki of 1975, as revised in 1983, and was approved by the Korean National Institute for Bioethics Policy (approval number: P01- 202206 -01- 016). Written informed consent was obtained from the patient for publication of the details of their medical case and any accompanying images.
KCS was coined for corneal topography with abnormal localized steepening over +47.00 D or an asymmetric bowtie pattern, a normal-appearing cornea on slit lamp biomicroscope, and at least 1 of the following signs: minor topographic asymmetry oblique cylinder greater than 1.50 D, central corneal thickness less than 500 µm, or clinical KC in the fellow eye [1-9]. Additionally, the increase with a positive sign of the posterior coma to 90° were presented on Scheimpfug pacido topography (Pentacam, Oculus, Wetzlar, Germany) [10].
Of patients with KCS who were treated at the Woori Eye Clinic between February 2019 and October 2020.Inclusion criterias in this study were 1. who under went L-LAK-CXL, 2. Who showed myopia of more than -1.0 diopter, 3. KCS manifesting both corneal focal steepening (Kmax) > +47.0 D and minor topographic asymmetry (SUM〉80 µm), 4. 20/20 in corrected vision, and 5. postoperative follow-up check over 1 year. Patients with follow-up examination under 1 year, history of other ocular operations or trauma, pregnancy or lactation, glaucoma, and causes of ocular astigmatism were excluded. The pre- and postL-LAK-CXL results were analyzed.
Patients with refractive errors underwent L-LAK using a 193-nm ISO-D 200 laser (Kera Harvest Inc., Taiwan). Laser correction was performed by the same surgeon (BM Min) using an identical method [15-20] for all patients. Local anesthesia was induced by instillation of 0.50% propacaine hydrochloride (Alcaine, Alcon NV, Vilvoorde, Belgium). For LASEK, a 9.0–9.5-mm diameter patch of corneal epithelium was removed with a brush. For refractive correction, laser ablation was performed in the 6.0 - 6.5 mm optic zone and more 2.0 mm transitional zone to correct myopia and astigmatism. To perform LAK [15-20], we used the Vision-Up software (WellC, Busan, Republic of Korea) to analyze the corneal deviations based on Orbscan II (Bausch & Lomb, Bridgewater, NJ, USA) corneal maps. These also served as predictors of corneal myopic change as a result of the removal of the thicker corneal regions, as
determined by LAK. Therefore, we were able to ablate the cornea to create central symmetry without changing the refractive power [15-20]. The following variables were analyzed: the pre- and postoperative (for L-LAKCXL); uncorrected distance visual acuity (UDVA), spherical equivalent (SE), sphere, cylinder, intraocular pressure (IOP), kappa angle on Orbscan map, central corneal thickness (CP), pupil size, SUM (µm), and distance between the maximum posterior elevation (best-fit-sphere [BFS]) and the visual axis (DISTANCE; mm). The refraction was measured using an auto refractometer/keratometer and was calculated as the SE.
UDVA was measured at a distance of 6 m, and was converted to the logarithm of the minimum angle of resolution (LogMAR). TBUT, tear osmolarity were measured with Keratograph 4 (Oculus, Germany).
Pre- and postoperative deviations in corneal thickness (SUM) and DISTANCE were analyzed using the identical method [15-20].
Surgical Technique of L-LAK-CXL
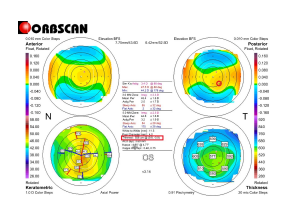
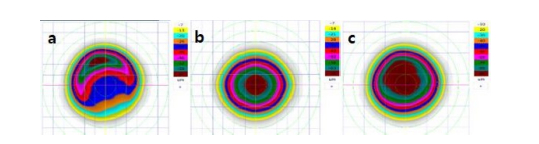
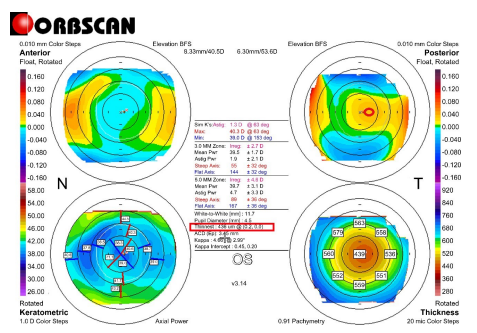
All patients were operated under administration. To perform corneal remodeling with L-LAK [15-20], we used the Vision-Up software (Well C, Busan, Republic of Korea) toanalyze the corneal deviations based on Orbscan II (Bausch & Lomb, Bridgewater, NJ, USA) corneal maps (Figure 1) to predict the amount of ablation on a thicker corneal region and to determine the direction of the axis (degree) (Figure 2a).
These also served as predictors of corneal myopic change as a result of the removal of the thicker corneal regions (customization ablation, Figure 2a), as determined by LAK. We operated original ablation for original refractive errors (Figure 2b) and customization ablation (Figures 2a) for both the thicker peripheral cornea and the central cornea to correct myopic shift due to LAK simultaneously with the same laser machine of a 193-nm ISO-D 200 laser (Kera Harvest Inc., Taiwan). Therefore, we were able to ablate the cornea to create central symmetry withoutchanging the refractive power (Figure 2c, and 3). Intraoperatively, optic zone (mm) in L- LAKwas 6.4, transitional zone (mm) was from 6.4 to 8.4.
CXL [21-23] was performed after L-LAK under the epithelium off state. 0.1% Riboflavin (10mg riboflavin-5-phosphate in 10 mL dextran-T-500 20% solution) (Vibe X: Avedro Inc., Waltham, MA, USA) was administered topically every 5 minutes for 30 minutes. Before UV irradiation, the surgeon confirmed that the riboflavin was fully absorbed into the corneal stroma by slit lamp inspection and the presence of a riboflavin flare in the anterior chamber. The cornea was exposed to UV light with a wavelength of 370 nm and irradiance of 3.0 mW/cm2 of UVA light (Avedro Inc., Boston, MA, USA) for a total time of 30 minutes, and then T-lens fitted. After close observation postoperatively, discharged. Topical antibiotic (Vigamox; Alcon, Fort Worth, Tx, USA) were instillated every 6 hour for 1 week, and steroid eye solution (Ocumetholone; Samil Pharmaceutical, Seoul, Republic of Korea) were instillated every 6 hour for 6 weeks.
Results
The age range of the patients was 23–40 years (average: 31.8 years). The male-to-female ratio was 1:1, follow up periods (months) were 18-30 (average 23.8). Follow up period (months) was from 18 to 30 (average 24) (Table 1).
Intraoperatively, optic zone (mm) was 6.4, ablation depth (µm) was 45–96 (average: 69) in the central cornea and 50-76(average 64) in peripheral cornea, myopic shift (diopters) due to LAK-SCAP was -1.25 – -1.75 (average: 1.50), residual stromal depth (µm) was 390–461 (average: 438) for L-LAK (Table 2).
For pre and postoperative findings (Table 3), SE (diopters) were -1.75 – -5.50 (average: - 3.44), but 0 – -0.50 (average: -0.34) after L-LAK-CXL, IOP and pupil size were similar between pre and postoperative. The UDVA (LogMAR) had increased after L-LAK-CAL (from an average of 0.93 to 0.00); hence, the L-LAK-CXL exhibited good outcomes for SE and UDVA. There were no cylindrical axial changes.
And the CP (µm) had decreased postoperatively (from an average of 581 to 508). In keratometry, Kmean and Kmax were decreased postoperatively (from 44.96 to 42.65 and from 48.00 to 43.88, respectively) (Table. 4).
Further, the sum of the corneal thickness deviations in four directions (SUM) and the distance between the maximum posterior elevation (best-fit-sphere [BFS]) and the visual axis (DISTANCE) decreased (from 165 to 63 µm, from 1.02 to 0.28mm, respectively) after the L-LAK-CXL. The angle kappa values were lowered after the L-LAK-CXL (Table 5).
TBUT was increased postoperatively (from 5.78 to 18.56 seconds in average), and tear osmolarity was decreased postoperatively (from 0.58 to 0.20 mOsmol/L in average) (Table 6). There was no corneal ectasia postoperatively.
Discussion
In this study, the SUM on Orbscan map and focal corneal steepening (Kmax) markedly decreased postoperatively, and SE and UDVA showed good outcomes and no corneal ectatic change after L-LAK-CXL. When the SUM on an Orbscan map is >80 µm (asymmetric cornea), corneal biomechanical interaction of corneal thickness, corneal stiffness and intraocular pressure causes the protrusion of regions of the cornea that have become thinner after the laser ablation easily, which steepens the cornea further, leading to ectasia [15-20,24-26]. With LAK, this parameter might be markedly decreased; in patients who underwent L-LAKCXL, the SUM (µm in average) was significantly decreased from 165, preoperatively to 63 postoperatively. Moreover, the reduction in DISTANCE (average) between visual axis center and thinnest point was changed from an average of 1.02 mm to 0.28 mm after L-LAK-CXL. It can be evidence that means to improvement in corneal symmetricity. So, we could correct the refractive errors in myopic patients with KCS without postoperative corneal ectasia [15-20].
In this study topography was assessed with an Orbscan map that can calculate SUM and the distance between the BFS and visual axis (DISTANCE). This method was quite useful for measuring the symmetry of the cornea centered on the visual axis [15-20]. But for detecting the earlier stage of KC, corneal aberrometry findings such as the posterior coma to 90° with Scheimpflug topography and focal epithelial thinning and epithelial thickness in the thinnest corneal zone with anterior corneal OCT are currently used as a indicater [27]. LAK could be executed exactly with the help of Vision-Up software (Well C, Busan, Republic of Korea) to analyze the corneal thickness deviations based on Orbscan II (Bausch & Lomb, Bridgewater, NJ, USA) corneal pachymatric maps, and to predict the amounts of ablation in a thicker corneal region, the direction of axis (degree), amounts of ablation, and corneal myopic change as a result of the removal of the thicker corneal regions. Therefore, we were able to ablate the cornea to create central symmetry without changing refractive power [15-20]. LAK could be new customization method15-20 to make symmetric cornea on KCS, additionally CXL made it keep well [21-23].
For focal corneal steepening (Kmax), the postoperative Kmax (average) was flatten to +43.88 diopters, compared that of the pre-L-LAK (+48.00 diopters), and also TBUTs (seconds in average) were markedly increased from 5.78 at pre-L-LAK to 18.56 at post-L-LAK-CXL. It may be expected that irregular cornea manifesting focal steepening cornea at pre-L-LAK-CXL could make the tear break easily, but postoperative even cornea could keep the tear layer well [28-30]. The relationship between corneal morphology and TBUT will be studied more in future. There are several limitations in this study. 1. Because L-LAK-CXL is a recently developed technology, we were able to follow up for short periods in only four patients with KCS; thus, more studies with longer follow-up times, with a large number of patients with KCS were needed, and 2. Changes of corneal dryness are required in the future to investigate the outcomes, including the stability of corneal symmetry and corneal curvature over time. 3. It is necessary to study various races only by studying only Koreans.
Conclusion
In conclusion L-LAK-CXL, a novel corneal remodeling technique, resulted in a decreased SUM and DISTANCE, increased corneal symmetry, and increased TBUT with good visual outcomes in a myopic patient with keratoconus suspect manifesting peripheral asymmetry of corneal thickness (a SUM of ≥80 µm) and focal corneal steepening (Kmax) over + 47.0 diopters
Conflicts of Interest
The authors declare that there is no conflict of interest regarding the publication of this paper.
Acknowledgments
We would like to thank for Rag Seon Han, Eun Mi Jang, Ji Yeon Choi, Mi Kyung Kim, Ji Suk Kwon, Hye Won Jung and Sun Hee Lee at the Woori Eye Clinic for assisting with the ocular examinations.
Ethics Statement
This study was conducted in accordance with the Declaration of Helsinki of 1975, as revised in 1983, and was approved by the Korean National Institute for Bioethics Policy (approval number: P01- 202206 -01- 016). Written informed consent was obtained from the patients.
Author contributions
Conceptualization: Byung Moo Min; Data curation: Byung Moo Min; Supervision: Byung Moo Min; Writing-original draft: Byung Moo Min; Writing-review & editing: Byung Moo min.
- Shi Y (2016) Strategies for improving the early diagnosis of keratoconus. Clin Optom (Auckl) 8: 13-21.
- Saad A, Gacinel D (2012) Evaluation of total and corneal wavefront high order aberration for the detection of forme fruste keratoconus. Invest Ophthalmol Vis Sci 53: 2978-92.
- Schlegel Z, Hoang-Xuan T, Gatinel D (2008) Comparison of and correlation between anterior and posterior corneal elevaton maps in normal eyes and keratoconus-suspect eyes. J Cataract Refract Surg 34: 789-95.
- Klyce SD (2009) Chasing the suspect: keratoconus. Br J Ophthalmol 93: 845-7.
- de Sanctis U, Arango V, Dalmasso P, Brusasco L, Grignolo F (2013) Diagnosis of subclinical keratoconus using posterior elevation measured with 2 different methods. Cornea 32: 911-5.
- Waring GO (1993) Normanclature for keratoconus suspect. J Refract Surg 9: 219-22.
- Vazirani J, Basu S (2013) Keratoconus: Current perspectives. Clin Ophthalmol 7: 2019-30.
- Li X, Yang H, Rabinowitz YS (2009) Keratoconus classification scheme based on videokeratography and clinical signs. J Cataract Refract Surg 35: 1597-603.
- Schlegel Z, Hoang-Xuan T, Gatinel D (2008) Comparision of and correlation between anterior and posterior corneal elevaton maps in normal eyes and keratoconus-suspect eyes. Surgery Cataract Refract Surg 34: 789-95.
- Feng K, Zhang Y, Chen YG (2021) The possible causes for tomography suspect keratoconus in a Chines cohort. BMC Ophthalmol 21: 47.
- Levy A, Georgeon C, Knoeri J, Tourabaly M, Levwziel L, Bouheraoua N, Borderie VM (2022) Corneal epithelial thickness mapping in the diagnosis of ocular surface disorders involving the corneal epithelium: A comparative study. Cornea 41: 1351-61.
- Randerman JB (2006) Post laser in-situ keratomileusis ectasia: Current understanding and future directions. Curr Opin Ophthalmol 17: 406-12.
- Roberts C (2000) The cornea is not a piece of plastic. J Refract Surg 16: 407-12.
- Roberts CJ, Dupps Jr WJ (2014) Biomechanics of corneal ectasia and biomechanical treatments. J Cataract Refract Surg 40: 991-8.
- Agudo JAR, Park J, Park J, Lee S, Park K (2009) Laser asymmetric ablation method to improve corneal shape. Lasers Med Sci 34: 1763-79.
- Min JS, Min BM (2020) Comparison between surgical outcomes of LASIK with and without laser asymmetric keratectomy to avoid conventional laser refractive surgery adverse effects. Sci Rep 10: 10446.
- Min JS, Min BM (2021) A novel approach to enhancement linked laser asymmetric keratectomy using semi-- cylindrical ablation pattern in patients with myopic regression after laser refractive surgery. Clin Ophthalmol 15: 1751-8.
- Min JS, Min BM (2021) Clinical outcomes of laser asymmetric keratectomy to management postoperative adverse effects-A retrospective clinical trial. The Open Opthalmol J 15: 171-7.
- Min JS, Min BM, Lee DC (2021) Laser asymmetric keratectomy using a semi-cylindrical ablation pattern to avoid adverse effects of laser refractive surgery. Austin J Clin Ophthalmol 8: 1120.
- Min JS, Min BM (2021) Comparison of outcomes of laser refractive surgery (LRS) alone and LRS with laser asymmetric keratectomy in patients with myopia: A retrospective study. Medicine (Baltimore)100: e25366.
- Galvis V, Tello A, Oretiz A Escaf L (2017) Patient selection for corneal collagen cross-linking: an updated review. Clin Ophthalmol 11: 657-68.
- Hersh PS, Greenstein SA, Fry KL (2011) Corneal collagen crosslinking for keratoconus and corneal ectasia: Oneyear results. J Cataract Refract Surg 37: 149-60.
- Mastropasqua L. Collagen cross-linking: when and how? A review of the state of the art of the technique and new perspectives. Eye Vision 2: 19.
- Ortiz D, Pinero D, Shabayek MH, Amalich-Montiel F, Alio JL (2007) Corneal biomechanical properties in normal, post-laser in situ keratomileusis and keratoconic eyes. J Cataract Refract Surg 33: 1371-5.
- Leccisoti A (2007) Corneal ectasia after photorefractive keratectomy. Graf Arch Clin Exp Ophthalmol 245: 869-75.
- Lee H, Roberts CJ, Kim TI, Ambrosio R Jr, Elsheikh A, Yong Kang DS (2017) Change in biomechanically corrected intraocular pressure and dynamic corneal response parameters before and after transepithelial keratectomy and femtosecond laser-assisted laser in situkeratomileusis. J Cataract Refract Surg 43: 1495-503.
- Castro-Luna G, Perez-Rueda A (2020) A predictive model for early diagnosis of keratoconus.BMC Ophthalmol 20: 263.
- Liu Z, Pflugfelder SC (1999) Corneal surface regularity and the effect of artificial tears in aquous tear deficiency. Ophthalmol 106: 939-43.
- Huang FC, Tseng SH, Shih MH, Chen FK (2002) Effect of artificial tears on corneal surface regularity, contrast sensitivity, and glare disability in dry eyes. Ophthalmol 109: 1934-40.
- Siyahkamari M, Asharlous A, Mirzajani A, Koohian H, Jafarzadepour E et al. (2022) Effect of dry disease on central corneal thickness and corneal topometric indices measured by Scheimflug tomography. Act Med Iran 12: 777-81.

Tables at a glance
Figures at a glance