Self-Medication among Patients in Ophthalmology at the National University Hospital Center - Hubert Koutoukou Maga in Cotonou Benin
Received Date: November 27, 2023 Accepted Date: December 27, 2023 Published Date: December 30, 2023
doi: 10.17303/jooa.2023.7.104
Citation: Abouki COA, Alfa BIA, Aigbe N, Holonou MAT, Assavedo CRA, Alamou S et al. (2023) Self-Medication among Pa tients in Ophthalmology at the National University Hospital Center - Hubert Koutoukou Maga. J Ophthalmol Open Access 7: 1-14
Abstract
Introduction: Self-medication is a global phenomenon and potential contributor to human pathogen resistance to antibiotics. This contributed to review focus on the self-medication of drugs, their use, its safety and reason for using it.
Study Design and Methods: Conducted at the University Ophthalmology Clinic of CNHU-HKM in Cotonou, the study was prospective, cross-sectional, descriptive, and analytical over three months. It included all patients practicing self-medication in ophthalmology. Data were collected via Kobocollect and analyzed with R. Quality control was performed, followed by bivariate analysis to establish associations using the Prevalence Ratio with 95% CI. Patient confidentiality was strictly maintained.
Results: Out of 501 ophthalmology patients, 44.1% practiced self-medication, mainly new patients (64.7%). Self-medication users had an average age of 45.61 years, with 60.2% being female, predominantly of Fon ethnicity (51.6%), and having a higher level of education (53.4%). Main consultation reasons included visual impairment (42.5%). Allergic conjunctivitis (20.4%), cataract (17.2%), and hypermetropia (11.8%) were the most frequent diagnoses. Non-pharmaceutical products constituted 67.8%, eye drops 50.7%, and antibiotics (gentamicin) 79.3%. Factors influencing self-medication included gender, age, reception quality, and knowledge of self-medication. New patients were 1.3 times more likely to use self-medication.
Conclusion: Improved knowledge and understanding about self-medication may result in rationale use and thus limit emerging microbial resistance issues.
Keywords: Self-Medication; Ophthalmology; Associated Factors; CNHU-HKM Cotonou
Introduction
Self-medication is a global phenomenon and potential contributor to human pathogen resistance to antibiotics. The adverse consequences of such practices should always be emphasized to the community and steps to curb it. Rampant irrational use of antimicrobials without medical guidance may result in greater probability of inappropriate, incorrect, or undue therapy, missed diagnosis, delays in appropriate treatment, pathogen resistance and increased morbidity. This review focused on the self-medication of drugs, their use, its safety and reason for using it [1]. It is a major public health issue in recent decades, globally and particularly in Africa. Self-medication is defined as the initiation of medical or non-medical treatment by the patient, on their own initiative and without a medical prescription [2]. It involves the use, without a medical prescription, of medications or other medicinal products considered as such and authorized for market release, with the possibility for patients to obtain assistance and advice from pharmacists [3].
Study Methods
Our study took place at the Eye Department of National Teaching University in Cotonou, Republic of Benin. It was a prospective and cross-sectional study with a descriptive and analytical purpose, from July 1st to September 30, 2023. The study was an exhaustive recruitment that included any outpatient attending the eye department of the teaching hospital at Cotonou in Republic Benin, who provided their informed consent to participate to the study and who met the selection criteria. The dependent variable was self- medication, consisting of several components such as self- diagnosis, self-prescription, and self-dispensation/consumption. Data collection was done using Kobocollect, and analysis was performed with the R software. Quality control of collected data was conducted, including the identification of aberrant, missing, inaccurate, and duplicate data. Bivariate analysis was performed to determine associations between self-medication and independent variables using the Prevalence Ratio (PR) followed by its 95% Confidence Interval [CI95%]. The significance threshold was set at 5% using the Chi-square test. The study was conducted with strict confidentiality measures to protect patient identity.
Results
The survey involved 501 ophthalmology patients during the study period.
Out of the 501 patients consulting during the study period, 221 resorted to self-medication, representing a frequency of 44.1%. Among the 221 patients who practiced self-medication, 64.7% were new patients.
Sociodemographic characteristics
In this study, the mean age was 45.61 ± 21.28 years, with a median age of 46 years for patients who practiced self-medication, ranging from 2 to 101 years. Thirteen percent (13%) were under 18 years old.
Females constituted the majority at 60.20%, with a sex ratio of 0.66. The fon ethnic group and related groups accounted for 51.6%, and 53.40% had a higher level of education. Only 5.40% of patients practicing self-medication had no formal education, and 49.80% traveled a distance between 10-20 km to reach CNHU-HKM.
The following table illustrates the distribution of patients who practiced self-medication based on their sociodemographic characteristics.
Clinical Aspects
Reasons for consultation
The reasons for consultation were primarily represented by visual impairment in 42.50% of cases, ocular redness in 14.90% of cases, and photophobia in 10.90% of cases. The following table illustrates the distribution of patients who practiced self-medication based on the reasons for consultation.
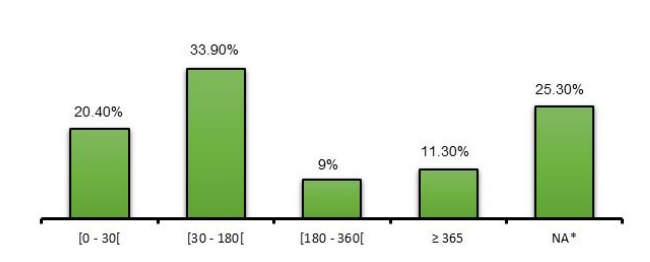
Onset of symptoms
Symptoms appeared between 30 and 180 days in 33.90% of the patients in the study who practiced self-medication in the ophthalmology department in 2023. Figure 1 illustrates the distribution of patients based on the onset of symptoms.
Diagnoses
Allergic conjunctivitis at 20.40%, cataract at 17.20%, and hypermetropia at 11.80% were the most diagnosed conditions among patients consulting in the ophthalmology department at CNHU-HKM and practicing self- -medication. Pterygium was found in 2 (0.90%) patients. One patient presented with retinal detachment, and three had ocular trauma.
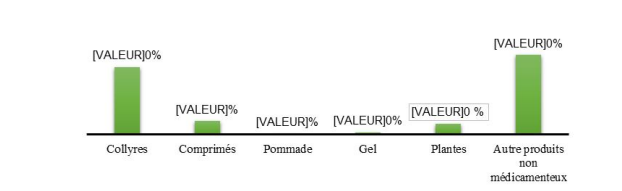
Therapeutic classes
In this study, non-pharmaceutical products were predominantly used by patients practicing self-medication in ophthalmology, accounting for 67.80%, including 8.10% for herbal remedies and 59.70% for other non-pharmaceutical products. Eye drops represented 50.70% of the products used (See the next figure).
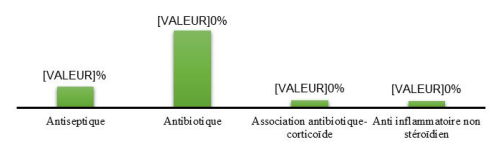
Among the 221 patients, 10% used antiseptics, with dacryo serum being the sole representation of this class, and 37.10% used antibiotics, with gentamicin eye drops being the most prevalent at 79.30%. The antibiotic-- corticosteroid and non-steroidal anti-inflammatory drug classes represented 3.60% and 3.20% of the pharmaceutical products used, respectively. The following figure illustrates the distribution of patients practicing self-medication based on the pharmaceutical classes of the medicinal products used.
Among the 221 patients, 50% used sugar water, and 38.90% used "kpatima" as the most prevalent types of non-pharmaceutical products (see the following table).
The majority of patients, 51.10%, who practiced self-medication in ophthalmology with pharmaceutical products obtained them from pharmacies, while 38.50% purchased their products from the market. The purchase intention came directly from the patient in 37.30% of cases.
Analysis of factors influencing self-medication practices Gender (p=0.006) and age (p=0.016) were found to influence self-medication. Specifically, patients under 30 years old had a 1.30 times higher chance of not practicing self-medication, while female subjects had a 1.32 times higher risk of self-medication compared to males.
There is a statistically significant relationship (p=0.005) between self-medication and the quality of patient reception in the ophthalmology department at CNHU-HKM in 2023. Poor reception quality increases the risk of resorting to self-medication in ophthalmology by approximately 1.34 times.
There is a statistically significant relationship between the practice of self-medication in ophthalmology and knowledge about self-medication (p=0.0001). The frequency of self-medication was 1.43 times higher in patients with no knowledge of self-medication compared to those with good knowledge of self-medication (PR=1.43, CI95% [1.18 - 1.74]). Knowledge about the consequences of self-medication was statistically associated with the practice of self-medication in ophthalmology (p=0.004). Patients with no knowledge of the consequences were 1.44 times more predisposed to self-medication in ophthalmology (PR=1.44; CI95% [1.10 - 1.89]).
Patients seemed to have a comprehensive understanding of self-medication at 38.97%. For them, self-medication solely involved pharmaceutical products available for purchase at the pharmacy or over-the-counter.
Among the 221 patients, 33.6% claimed to be aware of the consequences related to self-medication, and 100% of patients practicing self-medication believed that blindness was the feared consequence.
Over 80% of patients reported dissatisfaction after practicing self-medication.
Comparison of self-medication practices between former and new patients
The frequency of self-medication in ophthalmology among new patients was 1.30 times higher than that among former patients (PR=1.30; CI95% [1.05 - 1.60]). The following table illustrates the relationship between the practice of self-medication and the patient's tenure.
Discussion
In this study, the frequency of in-hospital self-medication is 44.10% in 2023. While this aligns with global figures ranging from 25.60% to 73.60% [4, 5], it surpasses rates found by Marquez et al [6] in Argentina, Gupta et al [7] in India, and Vonor et al [8] in Togo, which were 25.60%, 18.20%, and 29.50%, respectively. Our frequency markedly exceeds these studies, even though they were conducted on both general and in-hospital populations. This divergence may be explained by the inclusion of non-medicinal and unconventional products, prevalent in our region.
The mean age of patients in this study was 45.61±21.28 years, with extremes ranging from 2 to 101 years. The 40 to 60 age group predominated at 30.30%. These results are similar to those of Iyiade et al [8] in Nigeria, who found a mean age of 43.40 years with extremes of 2 months and 100 years, and the 31 to 50 age group predominating at 28.50%. However, they differ from Vonor et al [9] in Togo, where the mean age was 33.05±12.7 years, and the dominant age group was 20 to 30 years. Additionally, Shallam et al [10] in India found the 20 to 40 age group to be most represented at 40.60%, despite their studies being conducted in an intra-hospital setting. Pakitti et al [11] in Thailand reported the 15 to 24 age group as the majority at 67.50%, likely due to their sample being primarily comprised of high school and college students. Kyei et al [12] in Ghana, where the majority were young adults aged 18 to 35, constituting 50.80%, studied subjects aged 18 and above. Biska et al [4] in Malawi found the 30 to 39 age group to be the majority at 53.50%, possibly due to the selection based on adults aged 20 and above. Despite a higher proportion in the 40 to 60 age group in this study, these results, along with others, affirm that self-medication occurs across all age groups.
Females predominated at 60.20%, with a sex ratio of 0.66 in this study. During the survey, it was noted that the female gender was more representative of individuals resorting to self-medication. This inclination might be attributed to women's tendencies toward better self-care and a proactive approach in seeking remedies for prevention or healing. Similar patterns were observed by Marquez et al [6] in Argentina, where a female predominance was found at 57% with a sex ratio of 0.74, and by Kyei et al [11] in Ghana, reporting a female predominance at 56.80% with a sex ratio of 0.76. In contrast, Vonor et al [9] in Togo identified a male predominance with a sex ratio of 1.31, and Rajani et al [13] in India also found a male predominance at 65.50% with a sex ratio of 1.9. Despite the diverse proportions of women and men in the cited studies suggesting no apparent correlation between the patient's gender and self-medication practices, this study indicated that females were more prone to self-medication in ophthalmology.
The majority of patients resorting to self-medication belonged to the formal sector, constituting 56.60%, with 28.50% being civil servants and 28.10% students. The informal sector comprised approximately 43.40% of patients practicing self-medication in ophthalmology. These findings differ from those of Ajayi et al [8] in Nigeria, where the informal sector represented 44.20% of patients, the formal sector 27.70%, and 27% were students. Kyei et al [12] in Ghana reported that 78.40% of patients were in the informal sector, 15.90% were students, and 4% were civil servants. This variation could be explained by the study being conducted at CNHU, where formal sector workers receive comprehensive or partial healthcare coverage.
The majority of patients, 94.57%, who resorted to self-medication were educated, with 53.40% having a higher education level, 30.3% a secondary education level, and 10.90% a primary education level. The non-educated represented only 5.40% of cases. This percentage is higher than the results from Wangara [14] in Mali, where 68.13% of patients were educated. The education distribution was as follows: primary level 24.56%, secondary level 22.26%, higher level 21.30%, and non-educated 31.88%, despite the study being conducted in a hospital setting. Furthermore, according to Pakitti et al [11] in Thailand, university graduates comprised 53% of the sample, and university students constituted 35.50%. This discrepancy can be explained by their sample, which consisted of students and high school students. These diverse results demonstrate that self-medication is not dependent on the level of school attendance, even though the test is significant concerning this study.
Visual impairment at 42.50%, ocular pain at 12.20%, headaches at 12.20%, ocular redness at 14.90%, and photophobia at 10.90% were the most common reasons for consultation among patients resorting to self-medication in ophthalmology at CNHU-HKM. These results differ from those of Wangara [14] in Mali, where ocular pain and itching were the main symptoms leading to self-medication, accounting for 47.02% and 28% of cases, respectively. Shallam et al [10] in India found that redness was the primary symptom reported at 51.80%, followed by itching at 20.70%, and a foreign body sensation at 11.10%. In Thailand, according to Pakitti et al [11], dust in the eyes was the most cited reason at 55.50%, with ocular allergy symptoms such as itching, irritation, and tearing representing 18.50% of cases, ocular foreign bodies 16.50%, and dry eyes in contact lens wearers 9.50%. These varied results demonstrate that any ocular symptom can drive a patient to practice self-medication. There is no direct relationship between common ophthalmological symptoms and the practice of self-medication. It is noteworthy that during the study, 80.50% of patients reported dissatisfaction after self-medication in ophthalmology
It is well-known that the practice of self-medication can delay diagnosis and negatively impact the course of the underlying condition. In this study, allergic conjunctivitis at 20.40%, cataracts at 17.20%, and hypermetropia at 11.8% were the most diagnosed conditions among patients resorting to self-medication. According to Ajayi et al [8] in Nigeria, allergic conjunctivitis accounted for 22% of diagnoses, followed by refractive errors and senile cataracts at 20% each, and glaucoma at 13%. Marquez et al [6] in Argentina found that infectious and inflammatory pathologies were most common, representing 49.50% of diagnoses, followed by dry eye syndrome at 12.40%, and refractive errors at 11.30%. This variation can be explained by the symptoms reported by their patients. This study, along with those cited, did not establish a link between the patient's diagnosis and the practice of self-medication.
In this study, non-medicated products were most commonly used by patients resorting to self-medication in ophthalmology at 67.80%, followed by eye drops at 50.70%. Concerning non-medicated products, sugary water at 50% and kpatima, scientifically known as Newbouldia laevis, at 38.90%, were the most represented. These results differ from previous studies where eye drops were the most commonly found products. In Wangara's thesis [14] in Mali, eye drops represented 79.32% of the products used, and Vonor et al [9] in Togo reported a 94.10% utilization of eye drops. This discrepancy may be explained by beliefs in the therapeutic virtues of non-medicated products. In Benin, according to some patients in the study, "the use of sugary water on the eyes brings a certain satisfaction." A decoction made from Newbouldia laevis leaves is believed to treat ophthalmia and conjunctivitis [15]. According to the literature, only Newbouldia laevis has relevance in ocular pathology [16]. However, the modalities of using this plant are not clearly established. Moreover, patients do not seem to have sufficient information about the use of these non-medicated products. For instance, the use of lemon (citric acid) poses a risk to the eyes as it degrades corneal proteins by coagulating them to form a complex that hinders the penetration of the rest of the product into the eye.
Eye drops were the most representative for the proportion of medicated products. Among the cases recorded, 10% of patients resorting to self-medication in ophthalmology used antiseptic, and dacryoserum was the sole product representing this class. There were 37.10% of patients using antibiotics, with gentamicin eye drops being the most represented at 79.30% of this class. Hence, antibiotics were the most utilized pharmacological class. Our results are similar to those of Ajayi et al [8] in Nigeria and Shallam et al [10] in India, who found that antibiotics were the most represented, at 38.40% and 38.30%, respectively. This could be explained by the over-the-counter sale of antibiotics in eye drop form. In contrast, Marquez et al [6] in Argentina found that NSAIDs were the most represented class, accounting for 32%.
In this study, patients could identify the molecule or had empty containers to allow us to identify the molecule used. Most of them initially used non-medicated products purchased at the market or from a street vendor at 38.50% and 17.60%, respectively, at the beach at 13.60%, or from a relative at 8.10%. Those using medicated products obtained them from the pharmacy at 51.10%.
In the study sample, the initiative for self-medication came from the patient themselves at 37.30%, from a relative at 16.60%, and from a non-prescription healthcare professional, specifically the pharmacist, at 10%. However, there was a distinction between patients who voluntarily asked pharmacists for medications for a symptom and cases of pharmacy advice, which involves receiving medications under the advice of pharmacists or pharmacy vendors. Thus, our results and those of other previously cited studies affirm that pharmacists and their assistants play an important role in promoting self-medication worldwide [6]. It was also noticed that in some studies, patient guidance by pharmacists reduces the practice of self-medication [12]. According to Rajani et al [13] in India, of the 47.10% of cases received in the pharmacy, all were informed by the pharmacist to consult an ophthalmologist, and this was the reason for its low frequency.
However, if this is true for pharmaceutical products, it is not the case for non-medicated products. A study conducted in Malawi on traditional remedies revealed that the use of traditional remedies is widespread across the population and more common than resorting to allopathic drugs. Self-medication with traditional remedies is the means by which people, especially women, turn to in case of eye diseases [17]. Although patient guidance may reduce the risk of self-medication regarding pharmaceutical products, there is an urgent need to increase awareness of the consequences of using non-medicated products in ocular pathologies.
In this study, patients resorting to self-medication were mainly new patients. The frequency of self-medication in ophthalmology among new patients was 1.30 times higher than among returning patients. Our results differ from those of the aforementioned authors who did not compare self-medication practices based on patient status. However, Wangara [14] in Mali highlighted that 19.57% of patients resorting to self-medication had previously received a prescription from an eye care specialist, suggesting that these patients could be returning ones.
Moreover, if new patients engage in self-medication more than returning ones, it could be because returning patients have been sufficiently informed about the risks of self-medication during previous consultations.
Several sociodemographic factors significantly influence the recourse to self-medication. In this study, the female gender, previously mentioned, is implicated. This could be explained by the fact that women are more exposed to traditional and unconventional experiences.
Additionally, the new patient status was also a influencing factor in the practice of self-medication. However, the risk was lower for patients who had overall knowledge of the potential consequences of self-medication, while poor quality of reception increased the risk of resorting to self- -medication by 1.34 times.
These results differ from those of Wangara [14] in Mali and Kyei et al [12] in Ghana, who reported that economic factors and difficult access to healthcare were determinants in the practice of self-medication. On the other hand, Shallam et al [10] in India found that the availability of medications in pharmacies was the most mentioned factor by 30.40% of their patients, even though 11.70% cited economic reasons such as the high cost of consultations. However, Biska et al [4] in Malawi found that 76.80% of cases mentioned economic factors, particularly the high cost of medications prescribed by hospital practitioners. Thus, the results of this study and those of some authors imply that socio-economic status has an impact on the practice of self- -medication. This study strongly associates sociodemographic factors such as gender with the practice of self-medication.
Conclusion
There is need to augment awareness and implement legislations to promote judicious and safe practices. Improved knowledge and understanding about self-medication may result in rationale use and thus limit emerging microbial resistance issues.
- Al Balushi KA, Al Shibli S, Al Zakwani I (2014) Self- -medication: a current challenge. Journal of Basic and Clinical Pharmacy 5: 19-23
- Queneau P (1998) Self-prescription, self-medication, self-consumption of the elderly. Second APNET conference, Luxembourg. John Libbey Eurotext 134p.
- Edwards RS (1987) Ophthalmic emergencies in a district general hospital casualty department. Br J Ophthalmol 71: 938-42.
- Pouillard J (2001) Risks and limits of self-medication. Report to the Council of the Order of Physicians, Paris. 10-2.
- Bisika T, Courtright P, Geneau R, Kasote A, Chimombo L, Chirambo M (2010) Self-treatment of eye diseases in Malawi. African Journal of Traditional Complementary and Alternative Medicines 6: 23-9.
- World Health Organization (2008) Guidelines for the regulatory assessment of medicinal products for use in self- -medication, Genève. November 76p.
- Marquez GE, Torres VE, Sanchez VM, Gramajo AL, Fernando NZ, Peña Y et al. (2012) Self-medication in ophthalmology. A questionnaire-based study in an argentinean population. Epidemiol Ophthalmic. 09 Juillet 19: 236-41.
- Gupta N, Vashist P, Tandon R, Gupta SK, Kalaivani M, Dwivedi SN (2012) Use of traditional eye medicine and self-medication in rural India. A population-based study. Public Library of Science 12: 1-11.
- Ajayi A, Omotoye J, Ajite O, Fadamiro O, Ajayi E (2014) Self-medication practices among patients seen in a Suburbantertiary Eye Care Centre in Nigeria. Asian Journal of Medical Sciences 2: 85-90.
- Vonor K, Agbogbodo E, Salou M, Koffi D, Balo K (2022) Self-medication with ophthalmic drugs in pharmacies in Togo. International Journal of Pharmacy and Pharmaceutical Research 2: 129-35.
- Shallam A, Mendonca N (2017) Self-medication practices among patients attending ophthalmology opd in a tertiary hospital in mangalore. Inde. Journal of Dental and Medical Sciences 9: 11-3.
- Pakitti T, Pornanong A (2005) Self-medicated over the counter ophthalmic solutions in central Bangkok. The authors recruited sequentially 200. J Med Association Thai. 88: 44-5.
- Kyei S, Ocansey S, Abu E, Gyedu N (2014) Appraisal of the practice of ocular self-medication in cape coast metropolis. Ghana Optometry Reports 1: 1-2.
- Rajani K, Sudhir H, Ajay A (2011) Self-medication with over the counter ophthalmic preparations is it safe? International Journal Biology Medecine Research 2: 528-30.
- Wangara NA (2021) Self-medication during eye conditions in consulting patients. [Doctoral thesis]. Bamako, Mali: Faculty of Medicine and Odontostomatology.
- Ngasse Bwegne JGB, Ayina Ayina CN, Pagnangdé AHB, Etaga NB, Nzekuie OS, Ouedraogo MS et al. (2022) Newbouldia’s Laevis biological effects against metabolic syndrome components: A review. World Journal of Advanced Research and Reviews 16: 121-38.
- Giorgeta J (2020) Chemical in the eyes, what to do and what is the danger? Journal of Women in Science.
- Gagnon L (2000) Traditional remedies for the treatment of eye diseases in Malawi. In Malawi, eye diseases are common among rural populations. 1: 2.

Tables at a glance
Figures at a glance