Venous Sinus Stenting for Ocular Manifestations of Idiopathic Intracranial Hypertension:A Retrospective Study
Received Date: December 20, 2023 Accepted Date: January 20, 2024 Published Date: January 23, 2024
doi: 10.17303/jooa.2024.8.101
Citation: Tamir Regev MD, Liron Kravetz MD, Perach Osaadon MD, Eyal Walter MD, Ainat Klein MD et al. (2024) Venous Sinus Stenting for Ocular Manifestations of Idiopathic Intracranial Hypertension: A Retrospective Study. J Ophthalmol Open Access 8: 1-11
Abstract
Aims: To evaluate the efficacy of venous sinus stenting (VSS) for ocular manifestations of idiopathic intracranial hypertension (IIH) among patients who were either refractory to conventional medical treatment or presented with fulminant IIH.
Methods: We retrospectively identified all patients diagnosed with IIH who underwent VSS in the years 2015–2022 in Soroka University Medical Center, Israel. The main outcome measures were visual acuity, visual field function (expressed as mean deviation), grade of papilledema (based on the Frisén scale), and retinal nerve fiber layer (RNFL) thickness measured by spectral domain optical coherence tomography (SD-OCT). These measures were compared pre- and post-VSS.
Results: Twenty-five patients were eligible for analysis. Mean best corrected visual acuity (BCVA) pre-stenting was 0.26 (logMAR), which improved to 0.12 (log MAR) post-stenting. Mean RNFL thickness pre-stenting was 161 μm, which improved to 91.5 μm at 6 months’ post-stenting (p>0.001). All patients with papilledema demonstrated improvement, expressed as decreased RNFL thickness, with complete resolution documented by ophthalmoscopic evaluation in 17 patients (68%).Among the patients, 32% mean visual field deviation improved from -5.53dB to -4.98dB at 12 months post-stenting (p=0.52).
Conclusions: In our study cohort, VSS appeared to improve ocular manifestations among patients with refractory or fulminant IIH. Patients experienced minimal side effects and complications, despite undergoing an invasive procedure. Additional research is warranted to further determine the efficacy and safety of VSS in patients with IIH.
Keywords: Idiopathic Intracranial Hypertension (IIH); Cerebral Venous Sinus Stenting; Cerebral Sinus Stenosis;
Introduction
Idiopathic intracranial hypertension (IIH) is a syndrome of elevated intracranial pressure (ICP) more common in obese women of child-bearing age [1]. Symptoms include headaches, pulsatile tinnitus, transient visual obscurations, and diplopia. The main risk is varying degrees of vision loss resulting from papilledema, with some degree of permanent field loss occurring in up to 25% of cases [2]. While a debate exists on whether it is a cause or an outcome of IIH, over 90% of patients have stenosis along the transverse sigmoid sinus junction, either bilaterally or in one dominant sinus [3].
The main medical treatment for IIH patients with mild-to-moderate vision loss includes recommendation for weight loss and pharmacological management, usually with acetazolamide [2,4], which is a carbonic anhydrase inhibitor that reduces cerebrospinal fluid (CSF) production and lowers ICP. Topiramate is another effective medical treatment option, and in some cases, diuretics (mainly furosemide) are initiated. However, some patients are refractory to medical therapy, are intolerant to medications or present with vision- threatening fulminant IIH. In these cases, surgical interventions commonly used are optic nerve sheath fenestration or ventriculo-peritoneal shunting [5]. Both procedures are effective but carry inherent risks [6]. In 2003, Higgins et al [7] reported a new treatment option—cerebral venous stenting (CVS), as an alternative interventional therapy [8].
Although the medical treatment is well-described, has been used successfully for many years and was recently validated in a prospective study [4], the best treatment for progressive or more severe vision loss remains controversial and lacks clear guidelines. Despite the growing literature concerning CVS, most studies compared non-objective parameters regarding visual and neurological outcomes before and after CVS.
Optical coherence tomography (OCT) is a novel, reliable tool that objectively detects structural changes in the retina and allows for early detection of patients at high- -risk for permanent vision loss. It is a feasible, objective tool for assessing optic nerve edema and atrophy. This study used OCT imaging to evaluate the efficacy of CVS among patients with severe IIH to compare structural changes in the optic nerve before and after CVS, over a one-year period.
Materials and Methods
This retrospective review study included all patients who were diagnosed with IIH and underwent VSS at Soroka University Medical Center, in Beer Sheva, Israel during 2015 to 2022.
The research was approved by the local Institutional Review Board. Informed consent was not required due to the retrospective nature of the study.
Patients were diagnosed with IIH using the modified Dandy criteria [9]. Included were patients who were refractory or intolerant to standard medical therapy and were referred for and underwent venous sinus stenting.
Patients were defined as refractory to medical therapy if under treatment with acetazolamide or topiramate (or both) up to 2000mg per day acetazolamide or topiramate 50mg BID or maximally tolerated dose, had either persistent subjective symptoms such as headache, retro-orbital pain, transient visual loss, diplopia, tinnitus or visual deterioration, or objective worsening or persistent papilledema according to the Frisén score or OCT RNFL measurements, or progressive visual field (VF) loss.
Fulminant IIH was defined as acute VF loss within the central 5° with rapid worsening of vision over a few days to >6/20 at least in one eye, in the presence of papilledema [10].
Only patients with at least 12 months follow-up after the procedure were included.
Patients lacking a complete neuro-ophthalmological examination as a baseline before the procedure and at least two follow-up checkups after the procedure were excluded. Patients with prior CSF diversion procedures were also excluded.
Clinical Evaluation
Pre- and post- stenting data regarding visual function and optic nerve appearance were recorded.
All patients underwent a complete neuro-ophthalmological examination, which included visual acuity measurement, eye movements, relative afferent pupillary defect (RAPD), Ishihara color vision testing and a complete slit lamp examination. Optic disk edema was evaluated on dilated fundoscopy and graded using the Frisén grade score. Best corrected visual acuity (BCVA) was measured on a standard Snellen chart and converted to LogMAR scale for statistical analysis.
Visual field mean deviation (MD) was measured using Humphrey automated perimetry. RNFL thickness on OCT (Heidelberg model) was used as a surrogate marker to monitor changes in ICP and especially to help assess any changes in low grade papilledema.
Although normal RNFL thickness is usually set at 90-100 μm, papilledema was defined when RNFL thickness was ≥ 120 μm and with atrophy mean RNFL <79 μm.
Examination was done at baseline prior to VSS, as well as within one-week post-stenting, 1- to 3-months poststenting, and approximately every 3-months until 12 months post-procedure.
Catheter Venography
All patients treated with VSS had initially been found to have variations in transverse sinus anatomy on computer tomography venography (CTV) or magnetic resonance venography (MRV). A significant stenosis gradient was defined as a minimum of 7 mmHg pre-stenting.
Before the procedure, patients were treated with 7 days of 100 mg aspirin and 75 mg of clopidogrel once daily, except for two fulminant patients who had to be treated urgently. After transfemoral venous access was obtained, a guided catheter was advanced into the proximal segment of the dominant sigmoid sinus. The patient was treated with intravenous heparin during the procedure to keep an activated clotting time (ACT) over 250 seconds. A microcatheter was guided into the superior sagittal sinus and a precise stent was placed in eligible patients. If bilateral stenosis with a significant pressure gradient was found, the stent was placed on the side with the higher-pressure gradient.
Statistical Analysis
Categorical variables were described by proportion of available cases. Continuous variables were presented as mean ± standard deviation (SD), median, minimum, and maximum. The repeated measurements of clinical parameters, i.e., visual fields, papilledema Frisén score, OCT and RNFL thickness, taken at pre-post VSS for up to 12 months of follow-up were analyzed using mixed effect linear modeling. The clinical measurements were regressed over an indicator of the period and the effect of post- versus pre- period was expressed by the corresponding linear coefficient "b", along with its p-value. Repeated measurements of the same patients and measurements in both eyes were treated as clusters in the analysis. All statistical analyses were conducted using SPSS, version 25 (IBM Corp, Armonk, NY), and R software.
Results
During the study period, 25 patients who met the inclusion criteria were included. The cohort was comprised mostly of female patients (92.0%, 23/25), at an average age of 30.6 ± 10.0 years (Table 1). The average BMI was 32.3 ±5.12. Indications for the procedure included 4 patients with fulminant course, 7 were drug intolerant and 18 were refractory to medical therapy. The mean opening pressure at diagnosis was 357.1 ± 100.0 mmHg
Follow-up Data
Symptoms
At 3–6 months after VSS, headaches were resolved in 18 patients (72%), improved in 4, and persistent in 3. No patients had worsening of headache. Both patients with diplopia reported complete resolution.
15 of 16 patients (93%) with transient visual obscurations (TVO) reported resolution and 1 patient reported significant improvement. No patients reported worsening of any of these symptoms after stenting.
Of the 21 patients complaining of tinnitus, 19 (90%) reported resolution after stenting and 1 reported an improvement but not resolution.
Fifteen of 25 patients (60%) were able to discontinue acetazolamide. The remaining 40% were able to significantly decrease their daily dose.
Visual Acuity Examination
Mean BCVA before stent placement was 0.26 ± 0.71 log mar. Among 48 eyes, mean BCVA was 0.12 log mar ± 0.10, at 6-months post-stenting and 4 eyes worsened. The mixed linear model indicated 2% improvement throughout the entire follow-up period (b=-0.02, p=0.17).
Color Vision Testing
The average score on Ishihara plate testing was 14/15 pre-stenting and 14.5/15 post-stenting.
Visual Fields
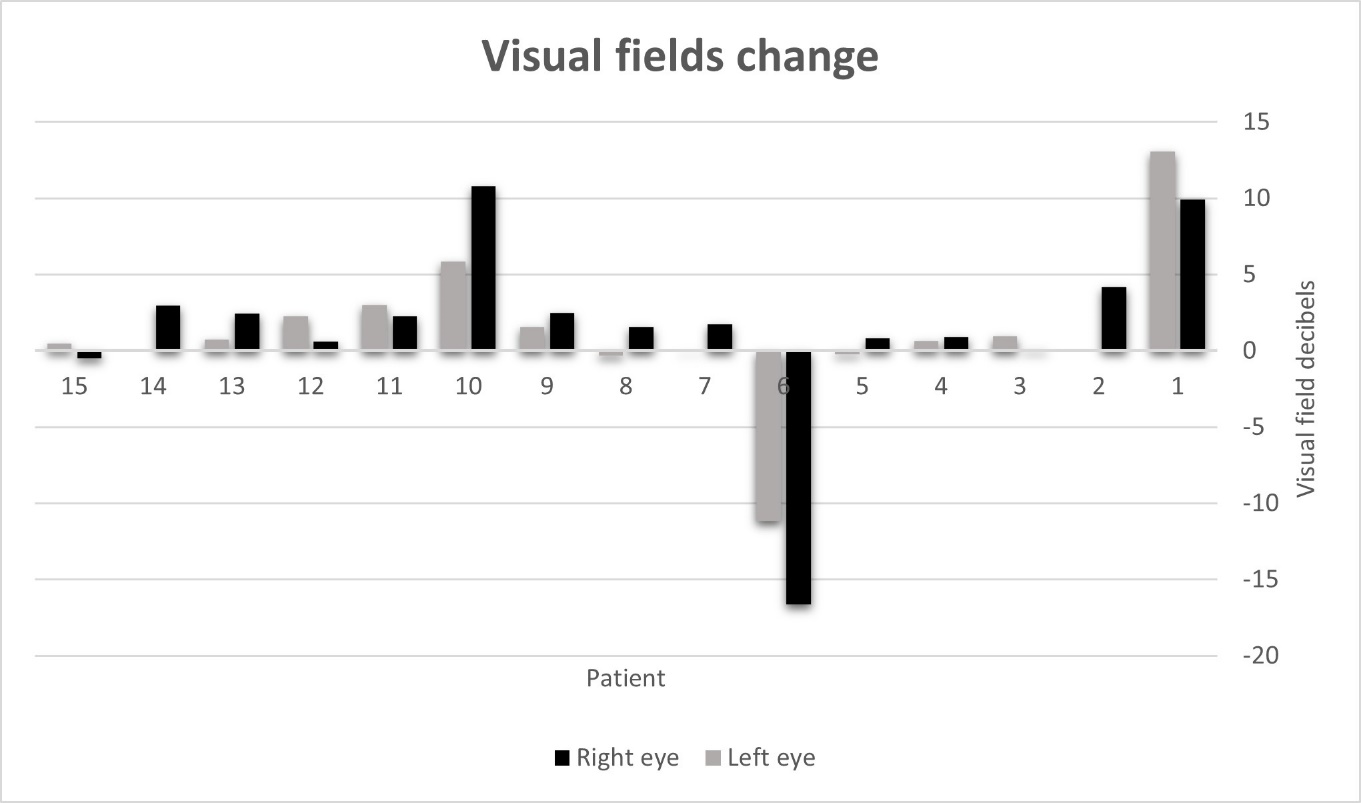
The average visual field was -5.29 ± 6.58 dB pre-stenting, and -4.48 ±7.62 d (post-stenting at the 6-month follow- up (Table 2), for both eyes. When divided into each eye, right eyes had a pre-stent value of -6.74 dB (b=-6.74, p<0.001) with 11% improvement during follow-up (b=0.11, p=0.68). Left eyes showed greater improvement of 24% (b=0.24, p=0.31). As shown in (Figure 2), 24 of 35 eyes improved, 2 eyes did not improve, and 9 worsened. In 1 eye with severe optic atrophy at presentation, MD improved from -8 to -3 dB.
Fundoscopy
Four eyes had optic nerve atrophy at presentation, which did not change after stenting.
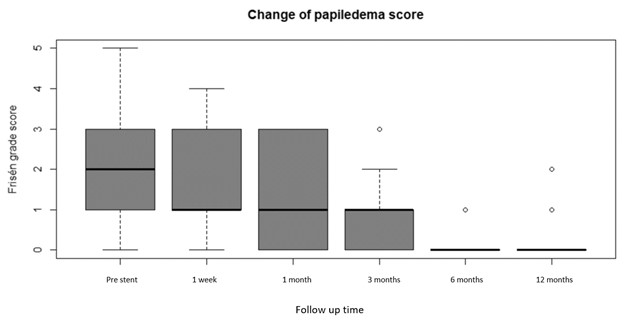
Forty-four of 46 (96%) eyes with papilledema showed improvement in mean Frisén grade from 2.21 ± 1.4 pre-stent to 0.22 ± 0.56) after 12 months of follow-up (b=2.57, p<0.001), with maximum change at 3-6 months post-stenting (Figure 1). In the linear mixed model (Figure 1), the decrease in papilledema according to Frisén grade score during the study follow-up was statistically significant (b=-0.43, p<0.001).
Spectral Domain Optical Coherence Tomography
Among 44 eyes, 42 (95.4%) demonstrated a reduction in the RNFL thickness following VSS (Table 2). Mean RNFL thickness 6 months post-stent was 91.5 ± 16.4 μm, decreasing from a pre-stent mean of (161 ± 93.3 μm) ( Table 3). Four eyes (9.9%) presented with generalized atrophy (mean RNFL 79 μm) before the procedure. Of which, 1 eye had progressive atrophy of another 18 μm at follow-up. Optic nerve atrophy did not develop in any patient after the procedure. RNFL thinning was not present at follow-up unless it was present at onset. In total, there was a 12% improvement during the follow up period (b=-0.12, p<0.001)
Subsequent Procedures
Of the 25 patients, only one required a secondary intervention. This patient underwent stereotactic ventriculo- peritoneal shunt placement approximately 6 months after the first procedure and underwent secondary stenting at 12 months due to headache and signs of progressive optic atrophy.
Tran’s sinus gradient Manometry Data from Catheter Venography
Average pre-stenting trans sinus gradient (TSG) was 18.53 mmHg (range 7-56 mmHg, median 17 mmHg). Post-stenting TSG was 2.75 mmHg (range 0-7 mmHg)
Complications of Stenting
Two patients experienced right groin hematoma at the puncture site, of which, 1 was treated with blood transfusion and was later discharged with complete resolution.
All patients underwent post-stenting CTV or MRV during the 3-12 months follow-up and none had restenosis.
Discussion
This retrospective study evaluated the efficacy of VSS in patients diagnosed with IIH who were refractory to medical therapy or with a fulminant presentation, mainly regarding ocular manifestations.
Patients were assessed based on pre- and post-stenting clinical parameters including papilledema (using the Frisén scale), RNFL thickening as demonstrated on SDOCT, VA and VF.
The pathophysiology behind IIH is poorly understood and has been subject to numerous research studies. Some of the proposed mechanisms include imbalance in CSF production/absorption and increased cerebral venous pressure [11]. None appears to be sufficient, as there seems to be a cycle of sinus stenosis and venous hypertension, further reducing CSF absorption, causing a rise in ICP and further worsening the venous stenosis. Regardless of these conflicting theories, it is apparent that venous stenosis has an important role in IIH progression, whether it is a cause or a result.
Our data show that patients experienced significant reduction in TSG after VSS. We believe this contributed to the reduction in ICP, leading to improvement in papilledema [12].
Similar to previous studies [13,14], the visual field improved after stenting. Most patients presented with varying degrees of visual field loss. Post-stenting, most showed overall some improvement in VF, with reduction in Frisén grade score of papilledema to grade 0, within weeks of stent placement. One patient had persistent VF loss associated with previous optic disc atrophy. Two patients with fulminant IIH had difficulty completing the VF test prior to stenting due to severe headaches, making the pre- and post-stenting comparisons less reliable.
In our cohort, the degree of visual loss correlated with the severity of disc edema: patients with more severe disc edema had more profound vision loss. This is a common and logical clinical course, that has been reported previously [15]. Nonetheless, it is important to note that patients with the highest grade of papilledema (grade 3 and above) exhibited the greatest improvement in VF testing post-stent.
RNFL OCT is used to quantify the thickness of the retinal nerve fibers. It is used as a bio marker for assessing optic disc edema as well, as it helps identify VF defects. In this cohort, all patients exhibited improvement in RNFL thickness, except those who presented with atrophy. The RNFL thickness was shown to decrease within the first week post-stenting, further supporting the assumption that the stenting directly resulted in ICP reduction, with improvement continuing up to 6 months. However, it is important to note that RNFL is also regarded as the sum of swelling plus atrophy [16], meaning that in some patients a greater decrease in thickness was observed only due to a previous state of severe atrophy.
As observed in previous reports, unilateral stenting of the transverse sinus was sufficient to reduce the pressure gradient, despite the presence of bilateral transverse sinus stenosis [17].
One of the greatest strengths of this study is that the same interventional radiologist performed the stenting in all patients, and all were followed by the same neurologist in the medical center.
Limitations
The retrospective nature of the study can introduce significant selection bias such as missing and incomplete data that could alter patient selection or miss other patients that should have been included, this is especially true regarding documentation of the ocular findings, as patients were treated by different neuro-ophthalmologists in various medical centers without a uniform history and examination. Additionally, the lack of guidelines for pre- and post-stenting testing may have also introduced an information bias. This is especially true regarding documentation of the ocular findings, as patients were treated by different neuro- ophthalmologists in various medical centers. The sample size was limited simply because this syndrome is rare, and few IIH patients require stenting as most are treated efficiently by oral medication.
All documented OCT RNFL were revised for correct layer segmentation. However, some of the scans could not be segmented due to limitations of the OCT machine in the presence of either extreme papilledema or severe atrophy upon reviewing of these scans manual segmentation could not be done due to layer morphology changes making it hard to distinguish between the different layers, using these patients data would have affected the results regarding those patients and the outcome and as such we decided not to use these scans.
Conclusions
IIH patients who are medically-refractory, medication- intolerant, or have a fulminant course can benefit from VSS. Post-stenting, most patients exhibited significant improvements in their symptoms, including reduction in headaches and tinnitus, as well as anatomical resolution of papilledema, to a degree enabling discontinuing chronic medical therapy. Although it is invasive, VSS appears to have an excellent safety profile with minimal complications, and while VSS is mainly used for IIH patients there is growing use of this technique in different populations such as patients suffering from pulsatile tinnitus, stenting for these patients helped in near resolution of their symptoms post the procedure, showing the greater potential of this procedure in the future.
Our results indicate that patients experienced considerable improvement in all categories evaluated, as documented in previous studies. The findings presented here add to the information from previous studies that this procedure is safe and effective. However, additional studies, including prospective interventional trials should be undertaken to further determine the efficacy and specific indications for VSS this future research may reveal a subset of patients that would favor from VSS and may alter patients’ life that could be seen as reduction of medication use and symptoms.
Acknowledgements
None
Financial Support
This research received no specific grant from any funding agency, commercial or not-for-profit sector.
Conflict of Interests
None
Ethical Standards
The authors assert that all procedures contributing to this work comply with the ethical standards of Israel on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008, and has been approved by the Institutional Ethics Committee of Soroka University Medical Center.
- Chen J, Wall M (2014) Epidemiology and Risk Factors for Idiopathic Intracranial Hypertension. Int Ophthalmol Clin 54: 10.1097/IIO.0b013e3182aabf11.
- Johnson LN, Krohel GB, Madsen RW, March GA (1998) The role of weight loss and acetazolamide in the treatment of idiopathic intracranial hypertension (pseudotumor cerebri). Ophthalmology 105: 2313-7.
- Ibrahim MH, Abo Zeid SH, Abd Elbar A (2014) Prevalence of venous sinus stenosis in Pseudotumor cerebri (PTC) using digital subtraction angiography (DSA). The Egyptian Journal of Radiology and Nuclear Medicine 45: 519-22.
- The NORDIC Idiopathic Intracranial Hypertension Study Group Writing Committee. Effect of Acetazolamide on Visual Function in Patients with Idiopathic Intracranial Hypertension and Mild Visual Loss: The Idiopathic Intracranial Hypertension Treatment Trial. JAMA. 2014; 311: 1641–51.
- Banta JT, Farris BK (2000) Pseudotumor cerebri and optic nerve sheath decompression. Ophthalmology 107: 1907-12.
- Vander Ark GD, Kempe LG, Smith DR (1971) Pseudotumor cerebri treated with Lumbar-peritoneal shunt. JAMA 217: 1832-4.
- Higgins JNP, Cousins C, Owler BK, Sarkies N, Pickard JD (2003) Idiopathic intracranial hypertension: 12 cases treated by venous sinus stenting. Journal of Neurology, Neurosurgery & Psychiatry 74: 1662-6.
- Kanagalingam S, Subramanian PS (2015) Cerebral venous sinus stenting for pseudotumor cerebri: A review. Saudi J Ophthalmol 29: 3-8.
- Friedman DI, Jacobson DM (2002) Diagnostic criteria for idiopathic intracranial hypertension. Neurology 59: 1492-5.
- Thambisetty M, Lavin PJ, Newman NJ, Biousse V (2007) Fulminant idiopathic intracranial hypertension. Neurology 68: 229-32.
- Donaldson JO (1981) Pathogenesis of pseudotumor cerebri syndromes. Neurology 31: 877-80.
- Schwarz J, Al Balushi A, Sundararajan S, Dinkin M, Oliveira C, Greenfield JP, et al. (2021) Management of idiopathic intracranial hypertension in children utilizing venous sinus stenting. Interv Neuroradiol 27: 257-65.
- Odago F, Smith J, Kedar S, Sudhakar P (2017) Visual Field Deficits in Patients with Headache Disorders: A 2-year Prospective Cohort Study (P1.192). Neurology. 88: 16.
- Ahmed RM, Wilkinson M, Parker GD, Thurtell MJ, Macdonald J, McCluskey PJ, et al. (2011) Transverse sinus stenting for idiopathic intracranial hypertension: a review of 52 patients and of model predictions. AJNR Am J Neuroradiol 32: 1408-14.
- Wall M (2010) Idiopathic Intracranial Hypertension. Neurol Clin 28: 593-617.
- Reid K, Winters HS, Ang T, Parker GD, Halmagyi GM (2022) Transverse Sinus Stenting Reverses Medically Refractory Idiopathic Intracranial Hypertension. Frontiers in Ophthalmology, 2.
- Larson A, Rinaldo L, Chen JJ, Cutsforth-Gregory J, Theiler AR, Brinjikji W (2021) Reductions in bilateral transverse sinus pressure gradients with unilateral transverse venous sinus stenting for idiopathic intracranial hypertension. J Neurointerv Surg. 13: 187-90.

Tables at a glance
Figures at a glance