Curcumin and Bromelain: An Effective Help to Subthresh old Micropulse Laser in Patient with Diabetic Macular Edema
Received Date: May 12, 2024 Accepted Date: June 12, 2024 Published Date: June 15, 2024
doi: 10.17303/jooa.2024.8.102
Citation: Mary Romano, Giovanna Vella, Andrea Garofalo, Luigi Petronella, Michele Tanturli, et al. (2024) Curcumin and Bromelain: An Effective Help to Subthresh old Micropulse Laser in Patient with Diabetic Macular Edema. J Ophthalmol Open Access 8: 1-10
Abstract
Diabetic macular edema (DME) represents the most common cause of sight loss in diabetic patients. It is characterized by swelling and thickening of the macula due to sub- and intra-retinal fluid accumulation in the macula, triggered by the breakdown of the inner blood-retinal barrier due to vessel glycosylation and inflammation. Therefore, antioxidant agents like nutraceuticals as adjuvant or prophylactic tools to standard therapies can become another weapon in the therapy of DME. Curcumin and Bromelain have shown in vitro and in vivo antioxidant, anti-inflammatory, and antiproliferative activity. This study aimed to explore the effectiveness of curcumin-based drugs in oral administration followed by SMLP in diabetic patients with clinically significant DME.
Methods: We enrolled 24 eyes, both naïve or not naïve, patients, older than 50 years old, with clinically significant DME and a central macular thickness (CMT) of 350 um or more measured by optical coherence tomography with a minimum follow-up of 6 months. Fifteen patients were assigned to subthreshold micropulse laser photocoagulation (SMLP); the other nine patients were assigned to subthreshold micropulse laser photocoagulation associated with oral administration of a curcumin-based drug.
Results: at the 4-month follow-up, the group of patients treated with sub- threshold micropulse laser associated with curcumin-based drug showed a lower mean CMT at OCT, compared to the group treated with laser alone. We found the same at the 6-month follow-up, with statistical significance.
Conclusions: Our study found no retreatment was necessary for patients who underwent SMLP and oral curcumin-based therapy. These patients experienced a significant decrease in CMT, confirmed at the OCT fovea B-scan at 4 and 6 months. Patients who underwent SMLP alone instead were found to have developed an increase in CMT, and retreatments were performed.
Keywords: Diabetes; Retinopathy; Macula Edema; Curcumin; Bromelain; Micro- pulse
Introduction
Diabetes is a widespread endocrinal pathology that is expected to affect an increasing number of people, from 578 million by 2030 to 700 million by 2045. [1] As far as ophthalmology is concerned, this increase in diabetic patients reflects an increase in diabetic retinopathy (DR) and its consequences, like diabetic macular edema (DME).
DME is the most common cause of sight loss in diabetic patients. It is characterized by swelling or thickening of the macula due to sub- and intra-retinal fluid accumulation triggered by the blood-retinal barrier breakdown [2]. DME begins with damage and pericyte loss, which induces early vascular alteration, leading to the formation of microaneurysms that cause fluid and serum recall at the base of diabetic macular edema.
Hyperglycemia induces obliteration of small vessels through glycosylation of the basement membrane of endothelial cells, causing retinal ischemia/hypoxia that leads to the release of proinflammatory cytokines and angiogenic mediators (3). The most crucial inflammatory factor linked to hypoxia and released from the early stages of diabetic retinopathy is the Vascular Endothelial Growth Factor (VEGF) [2,3]. It induces the loss of tight junctions in the retinal vessels, with consequent capillary perfusion defect and increased permeability [3]. Therefore, the use of agents that can reduce inflammation and neovascularization can reasonably contribute to the improvement of the postoperative clinical picture, just as it has been shown to happen with the use of intravitreal therapies with steroids or anti-VEGF drugs [4]. In addition to the conventional therapies of DME (Intravitreal Therapies; Laser Therapy; Subthreshold Micropulse Laser Photocoagulation), a new possibility for the future treatment of DME, is represented by the use of antioxidants. A central role in the pathogenesis is played by oxidative stress caused by hyperglycemia [5]. Reactive oxygen species such as H2O2 and superoxide anion are increased in the retina of patients with DME, inducing cellular damage and the production of various nuclear factors, such as NF-κB, which promote the expression of VEGF and other proinflammatory mediators, like ICAM-1, vascular cell adhesion molecule-1 (VCAM-1), monocyte chemotactic protein-1 (MCP-1), and cyclooxygenase-2 (COX-2) [6,7].
COX-2 increases the synthesis of prostaglandins that stabilize hypoxia-induced factor-1 (HIF-1), which favors VEGF expression and NF-κB activation for COX-2 expression. This way, an inflammatory mediator loop is formed [8].
Therefore, antioxidant agents like nutraceuticals as adjuvant or prophylactic tools to standard therapies can become another weapon in the therapy of DME. Since 2013, reviews have been available on Curcumin and its potential as a therapeutic agent in retinal diseases [9,10]. There is much evidence in vitro and in vivo (experimental models) of Curcumin's antioxidant, anti-inflammatory, and antiproliferative activity (10). The anti-inflammatory action is carried out through multiple mechanisms: 1) increased production of endogenous steroids for action on the adrenal cortex; 2) inhibition of hepatic cortisone metabolism, increasing circulating steroids; 3) inhibition of activation of the proinflammatory transcription factor NF-kB 4) inhibition of interleukin and TNFα production (10). Furthermore, curcuminoids exert their antioxidant action through a scavenging effect of reactive oxygen species, such as superoxide anions and hydrogen peroxide, inhibiting lipid peroxidation and LDL oxidation [10]. Moreover, the possible anticarcinogenic activity of curcuminoids could be explained by some mechanisms such as inhibition of angiogenesis, an increase in the frequency of apoptosis, interference with some signal transduction modes, which are critical for cell growth and proliferation, inhibition of cyclooxygenase (COX) and lipooxygenase (LOX) [10].
Another absorbing nutraceutical agent is Bromelain. Much evidence in vitro and in vivo indicates the possible use of Bromelain in the therapeutic field [11,12]. Studies show that the use of supplements in combination with Bromelain, due to its neuroprotective, anti-inflammatory, and antioxidant role, including the ability to protect against hypoxia and angiogenesis, allows protection in the management of retinopathies such as DR and DME [13,14].
Furthermore, studies demonstrate that the perfusion of choroidal blood flow positively influences it [15]. It is a proteolytic enzyme with anti-edema and protective properties towards vitreous collagen fibers [13].
However, the most significant effect is that it is anti-inflammatory, facilitating the rebalancing of inflammation mediators (16,17). The mechanisms of the supposed anti-inflammatory action of Bromelain are the following: reduces the activation of COX-2 and PGE-2; stimulates the production of IL-1, TNF, IL-6, and INF; decreases the presence of Substance P and PGE-2 in the exudate; modulates the expression of CD44; activates Natural Killer cells and increases Il-2 secretion; and reduces the activity of T-helper cells [18-20].
Moreover, it induces fibrinolysis, reduces clotting capacity, reduces pre-kallikrein, factor X, prothrombin, and inhibits the production of bradykinin [20,21].
Considering this experimental evidence and the results of clinical experience has been hypothesized the usefulness of conducting a study in which we have tried to evaluate the effect of the nutraceuticals as adjuvant in patients affected by DME treated with Subthreshold Micropulse Laser Photocoagulation (SMLP). We report preliminary results of curcumine and bromeline effects in patients treated with SMLP.
Materials and Methods
Based on additional studies in the literature, such as the one by Chiosi et al [13] regarding the potential benefits of nutraceuticals in treating diabetic macular edema, we undertook a spontaneous uncontrolled study at the IRCCS Istituto Clinico Humanitas Eye Center in Milan, Italy.
We have analyzed 24 eyes, both naïve or not naïve, affected by clinically significant DME and treated with Subthreshold Micropulse Laser. Inclusion criteria are as follows:
- Men/women aged between 50 and 75 years
- Established type 2 Diabetes Mellitus diagnosis, under therapy with anti-hyperglycemic drugs
- Diabetes duration for at least eight years and not exceeding 15 years
- Absence of systemic complications of diabetes
- The last two HbA1c measurements before enrolling not exceeding 7.5%
- Best Corrected Visual Acuity (BCVA) ≥ 3/10
- Central Macular Thickness (CMT) between 350 um and 499 um measured by optical coherence tomography (OCT)
- Absence of other diseases of the macula (e.g., exudative macular degeneration, uveitis, ocular inflammation, epiretinal membrane, etc.)
- Absence of previous ocular surgery
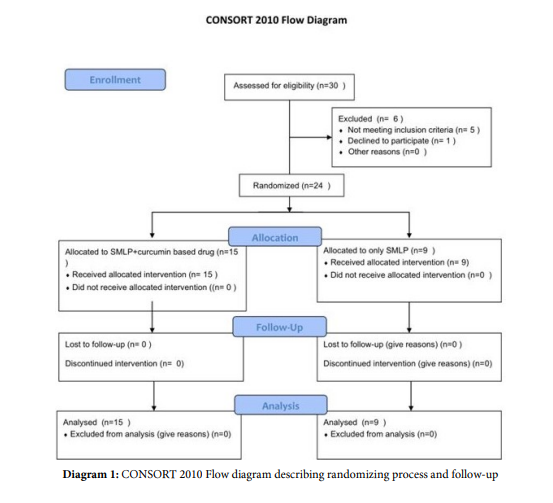
We treated the 24 patients in a completely randomized way (see diagram 1):
Let us say we did subthreshold micropulse laser photocoagulation (SMLP) in 15 patients, while the other 9 patients had been treated with subthreshold micropulse laser photocoagulation associated with oral administration of a curcumin-based drug (see Table 1).
The second group received before meals a tablet containing a fixed combination of Curcumin (200 mg), Artemisinin (80 mg), Bromelain (80 mg), and Black pepper (2 mg) for six months (Intrav it®, OFFHEALTH Spa, Firenze, Italy). The treatment scheme provided that a tablet was taken twice a day for the first month and once a day for the remaining five months.
The second group received before meals a tablet containing a fixed combination of Curcumin (200 mg), Artemisinin (80 mg), Bromelain (80 mg), and Black pepper (2 mg) for six months (Intrav it®, OFFHEALTH Spa, Firenze, Italy). The treatment scheme provided that a tablet was taken twice a day for the first month and once a day for the remaining five months.
The SML therapy was applied confluently to the macular area using three 7 × 7 spot grids with zero-spot spacing above and below the fovea (500 μm from its center) and one 7 × 7 spot grid with zero-spot spacing at each side (temporal and nasal) of the fovea (500 μm from its center).
Before administering SML treatment, laser titration was performed using the continuous-wave mode, a 200-μm spot, and a 200-ms exposure duration.
An area of edematous retina of > 2 disc diameters from the foveal center (if possible) was used for titration. The threshold power was determined by increasing the laser power in 10-mW increments, starting from 50 mW, until a barely visible tissue reaction was seen. As soon as this threshold was determined, the laser was switched to micropulse mode at a 5% duty cycle, and the laser power was adjusted to 4 times the continuous-wave threshold power (e.g., if a barely visible reaction was seen at 70 mW using continuous-wave power, then micropulse laser was applied with 280 mW). The SML therapy was then delivered using a 5% micropulse duty cycle, 200-μm spot, and 200-ms exposure duration.
An investigator performed at time 0, after 4 and 6 months of follow-up, the following examinations: BCVA, fundus examination, and Spectralis SD-OCT (Heidelberg Engineering GmbH, Heidelberg, Germany).
Central macular thickness was measured with dense high-definition fovea-centered cross-line B-scan. In the investigator's opinion, SMLP could be repeated each time if DME persisted, and such treatment was warranted, according to the presence of increased CMT on OCT or significant macular edema.
The statistical analyses were conducted to explore differences between control and treated patients. Continuous variables were reported as mean ± standard deviation (sd) or median ± Interquartile Range (IQR) with p values obtained from paired t-test with Holm correction for P values or Wilcoxon test, respectively.
The analyses were conducted separately for control and treated patients. Missing data at month six were handled using Last Observation Carried Forward (LOCF) using values from month 4 to create a new set of measurements. P < 0.05 was considered statistically significant.
The statistical analysis was performed with the R software version 4.3.2 - R Core Team (2023)._R: A Language and Environment for Statistical Computing_. R Foundation for Statistical - Computing, Vienna, Austria. https://www.R-project.org/
Results
We analyzed the CMT of 24 eyes affected by DME, of which 15 were treated with subthreshold micropulse laser photocoagulation + curcumin-based drugs, comparing them with the CMT of 9 eyes treated only with micropulse laser photocoagulation. The two groups were similar and comparable in demographic (age and sex) and ocular characteristics (see Table 1).
At time 0
The group treated with laser + Curcumin showed a mean (SD) of CMT measured by OCT of 414.13 (48.82) and a median [IQR] of 425.00 [391.00, 444.50] at time 0 from the start of the associated treatment. A similar measure was found in the control group, with a baseline mean (SD) of CTM of 396.67 (73.21) and a median [IQR] of 410.00 [395.00, 430.00].
O At four months: Calculating the CMT of the two groups at four months, we obtained that the group treated with laser + Curcumin showed a mean (SD) of CTM at 345.38 (56.16) and a median [IQR] of 370.00 [307.00, 386.00]. Instead, the control group treated only with micropulse laser showed a mean (SD) of CTM at four months of 404.88 (24.99) and a median [IQR] of 400.00 [395.00, 419.25]. The P- value was statistically significant (see Table 2).
At 6 months
Analyzing the values at 6 months, the laser + curcumin group presented a mean (SD) of CTM of 320.40 (72.69) and a median [IQR] of 312.00 [277.50, 363.50].
Instead, the control group treated only with micropulse laser showed a mean (SD) of CTM at 6 months of 373.33 (30.55) and a median [IQR] of 380.00 [360.00, 390.00]. The P- value was statistically significant (see Table 3).
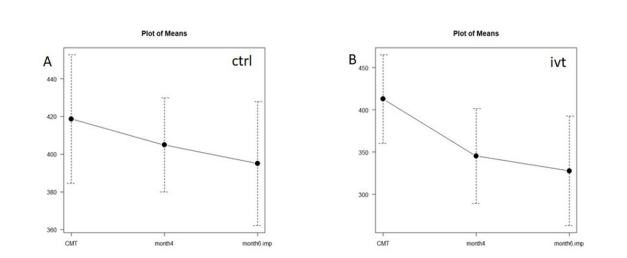
In The figure 1 and figure 2 we can observe the mean ± standard deviation of CMT over the follow-up period (base-line, month four and month six) in control (ctrl) patients (plot A) (p = 0.08) and treated (ivt) patients treated (plot B) (p =0.00016). A statistically significant CMT mean (SD) reduction was recorded in the treated groups after four months and a further reduction after 6 months.
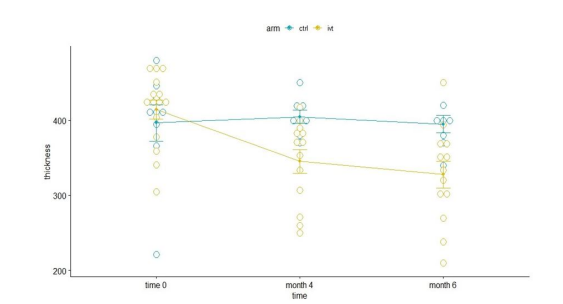
In figure 3 it is shown the comparison between the mean ± SD at baseline and after 4 and 6 months in the control (ctrl) group (green) and in treated (ivt) group (green) of the central macular thickness. The statistical analysis was performed using ANOVA for repeated measures to analyze the effect of the treatment and of the time.The P-value was 0.000056, so statistically significant.
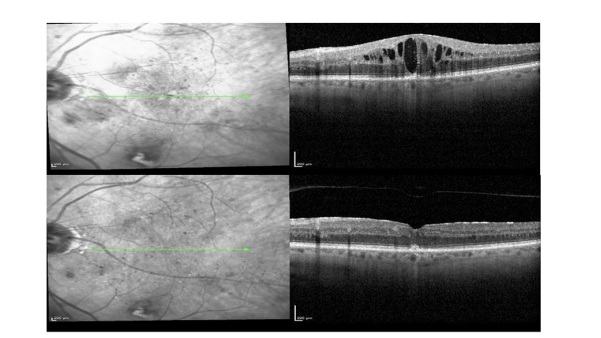
In figure 4, there is shown a macular OCT of a patient at time 0 and 6 months after the start of therapy with subthreshold micropulse laser photocoagulation + curcumin-based drugs. A complete reabsorption of the cystic macular edema was recorded, with the re- appearance of the physiological foveal depression and the reduction of the CTM.
Discussion
As far as diabetic retinopathy (DR) is concerned, glycemia high blood levels induce oxidative stress pathways and promote free radicals that are the leading cause of diabetic vascular syndrome onset. On the other hand, there is multiple pieces of evidence in vitro and in vivo of the pleiotropic role of Curcumin and Bromelain involved in the anti-inflammatory, antiproliferative activity, and anti-oxidative pathways in retinal tissues. Bromelain demonstrates anti-inflammatory properties akin to non-steroidal anti-inflammatory drugs, reducing plasma fibrinogen, increasing fibrinolytic activity, and decreasing bradykinin levels, all vital for controlling edema. Curcumin, artemisinin, bromelain, and black pepper each offer distinct therapeutic advantages for retinal diseases. Research has shown Artemisia to reverse conditions such as iris and retinal neovascularization, macular edema, vascular dilation, tortuosity, and fluorescein leakage when injected intravitreally in animal models like rabbits and monkeys. This evidence underscores artemisia's potential as an antiangiogenic treatment for diabetic retinopathy, as it helps regulate mitochondrial function and manage oxidative stress. Moreover, black pepper and its active ingredient, piperine, have been observed to modulate and reduce high levels of inflammatory biomarkers, including IL-1β, TNF-α, NF-κB, and malondialdehyde (MDA), in diabetic mice models. Therefore, this is why these antioxidants could represent another weapon in the therapy of DME.
Our study aimed to explore the effectiveness of oral administration of curcumin-based drugs followed by SMLP in diabetic patients affected by DME.
Preliminary results from this study demonstrated that the addition of a fixed combination of Curcumin (200 mg), Artemisia (80 mg), Bromelain (80 mg), and Black pepper (2 mg) to the standard therapy with subthreshold micropulse laser photocoagulation could improve the treatment of EMD in patients affected by type 2 Diabetes Mellitus
We found that patients who had undergone SMLP and oral curcumin-based therapy experienced a more remarkable and statistically significant decrease of CMT compared to the control group, confirmed by OCT fovea B-scan at 4 and 6 months. Four months after starting curcumin-based therapy + SMLP, they showed a statistically significant reduction of mean CMT of 16,6%, whereas we recorded an increase of the CTM in the control group. This difference was found to be even more marked at month 6, showing a statistically significant reduction of 20% of the CMT mean in the treated group as compared to the reduction of 0.4% in the control group. No relevant side effects were observed in patients assuming curcumine-based drugs.
Moreover, as a result of this marked reduction of CMT, we found that no retreatment was necessary for patients who had undergone SMLP and oral curcumin-based therapy, unlike patients who received only SMLP, many of whom needed to undergo retreatment. Therefore, curcumin-based drugs are not only an adjuvant that can increase the effectiveness of the laser in reducing macular edema in diabetic patients but also could improve the stability of outcomes, reducing the likelihood of retreatments.
Conclusion
The findings of this initial study indicate a potential positive impact of nutraceutical antioxidants such as Curcumin and Bromelain as dietary complementary supplements in the management of DME in patients with type 2 diabetes. This combination has the potential to enhance the effectiveness of conventional therapy and decrease the likelihood of requiring retreatment, thereby potentially serving as an additional therapeutic approach for DME in the future. Our ongoing efforts involve the continued enrollment of new patients to assess the long-term efficacy of curcumin-based medications and to validate the findings obtained.
Conflict of Interests
The authors declare no conflict of interest
- Verma AK, Goyal Y, Bhatt D, Dev K, Alsahli MA, Rahmani AH, Almatroudi A (2021) “A Compendium of Perspectives on Diabetes: A Challenge for Sustainable Health in the Modern Era.” Diabetes Metab Syndr Obes. 14: 2775-87.
- Romero-Aroca P, Baget-Bernaldiz M, Pareja-Rios A, Lopez-Galvez M, Navarro-Gil R, et al. (2016) “Diabetic macular edema pathophysiology: Vasogenic versus inflammatory.” J. Diabetes Res. 2016: 2156273.
- Zhang X, Zeng H, Bao S, Wang N, Gillies MC (2014) “Diabetic macular edema: new concepts in patho-physiology and treatment. Cell Biosci." 4: 27.
- Browning DJ, Stewart MW, Lee C (2018) Diabetic macular edema: Evidence-based management.” Indian J Ophthalmol. 66: 1736-50.
- Alfonso-Muñoz EA, Burggraaf-Sánchez de Las Matas R, Mataix Boronat J, Molina Martín JC, Desco C (2021) “Role of Oral Antioxidant Supplementation in the Current Management of Diabetic Retinopathy.” Int J Mol Sci. 22: 4020.
- Behl T, Kotwani A (2015) “Exploring the various aspects of the pathological role of vascular endothelial growth factor (VEGF) in diabetic retinopathy.” Pharmacological Research, 99: 137-48.
- Homme RP, Singh M, Majumder A, et al. (2018) “Remodeling of retinal architecture in diabetic retinopathy: disruption of ocular physiology and visual functions by inflammatory gene products and pyroptosis.” Frontiers in Physiology. 9: 1268.
- Lukiw WJ, Ottlecz A, Lambrou G, et al. (2003) “Coordinate activation of HIF-1 and NF-κB DNA binding and COX-2 and VEGF expression in retinal cells by hypoxia.” Investigative Opthalmology & Visual Science. 44: 4163-70.
- Wang LL, Sun Y, Huang K, Zheng L (2013) “Curcumin, a potential therapeutic candidate for retinal diseases.” Mol Nutr Food Res. 57: 1557-68.
- Menon VP, Sudheer AR (2007) “Antioxidant and anti-inflammatory properties of curcumin.” Adv Exp Med Biol 595: 105-25.
- Rathnavelu V, et al. (2016) “Potential role of bromelain in clinical and therapeutic applications” (Review). Biomed. Rep.
- Bitange Nipa Tochi et al. (2008) “Therapeutic Application of Pineapple Protease (Bromelain): A Review” Pakistan Journal of Nutrition, 7: 513-20.
- Flavia Chiosi et al. (2022) “Effect of a Fixed Combination of Curcumin, Artemisia, Bromelain, and Black Pepper Oral Administration on Optical Coherence Tomography Angiography Indices in Patients with Diabetic Macular Edema.” Nutrients, 14: 1520.
- Bassirou AM. Mounirou et al. (2022) “Diabetic Retinopathy: An Overview of Treatments.” Indian Journal of Endocrinology and Metabolism, 26: 2.
- Rossella D’Aloisio et al. (2022) “Choroidal Changes in Blood Flow in Patients with Intermediate AMD after Oral Dietary Supplement Based on Astaxanthin, Bromelain, Vitamin D3, Folic Acid, Lutein, and Antioxidants” Medicina, 58: 1092.
- Chakraborty AJ, et al. (2021) “Bromelain a Potential Bioactive Compound: A Comprehensive Overview from a Pharmacological Perspective.” Life (Basel). 11: 317.
- Newsletter Dighe et al. (2010) “Bromelain A Wonder Supplement: A Review” Pharmacology online, 1: 11-8.
- Jing-Rong Huang et al. (2008) “Bromelain Inhibits Lipopolysaccharide-Induced Cytokine Production in Human THP-1 Monocytes via the Removal of CD14.” Immunological Investigations, 37: 263-77.
- Rajendra Pavan et al. (2012) “Properties and Therapeutic Application of Bromelain: A Review” Biotechnology Research International, 2012: 976203-6.
- L. Ferrara et al. (2009) “Impiego Degli Enzimi Vegetali Nell’alimentazione E Nella Terapia.” Progress in Nutrition, 11: 4.
- Bharat Kwatra (2019) World Journal of Pharmacy and Pharmaceutical Sciences, 8: 11.

Tables at a glance
Figures at a glance