Refractive Errors and Effective Refractive Error Coverages Among Elementary School Children in Katsina State, Nigeria
Received Date: December 06, 2024 Accepted Date: January 06, 2025 Published Date: January 09, 2025
Citation: Muhammad M Rabiu, Manal O Taryam, Muhammed Nasiru, Ahmed Abubakar, Abduljalil Abdullah, et al. (2025) Refractive Errors and Effective Refractive Error Coverages Among Elementary School Children in Katsina State, Nigeria. J Ophthalmol Open Access 9: 1-11
Abstract
Purpose: To measure the prevalence of refractive error and effective refractive error coverage (eREC) among elementary students in Katsina state, Nigeria, a cross-sectional school-based survey was conducted.
Patients and Methods: A two-stage cluster random sampling technique was used to select 2,300 students in 194 elementary schools in Katsina state. In the first stage, 20 schools were randomly selected by probability proportional to size. In the second stage, one class each from classes one and six arms of each school were randomly selected. All students in selected classes were included in the study. Each student had uncorrected visual acuity tested for each eye and with glasses if worn. Eyes with a presenting vision of less than 6/12 had pinhole vision tested. They all underwent noncycloplegic autorefractometry and eye examination.
Results: A total of 2224 students out of 2335 enumerated were examined (95.2%). Half were boys, and 49.9% were from class one. Only 0.4% and 1.1% of the students in classes one and six, respectively, had vision impairment.
Among class six students, the prevalence of hypermetropia and myopia was 2.0% and 20%, respectively, while for class one, it was 1.1% and 10.9%, respectively. The eREC (person) was 33.3% and 0% for classes six and one, respectively. However, the effective clinical refractive error coverage (person ) which provides the coverage of refractive error services based on routine clinical practices was only 10% for class six and 0% for class one. The effective Glasses ‘need’ which gives the percentage of persons that could be improved with glasses was 0.9% and 0.2% for classes six and one respectively.
Conclusion: The eREC in Katsina state is low even as the need for refractive error services seems low. In addition to eREC as an indicator to monitor refractive error services, the eCREC may be a more useful and practical indicator.
Keywords: Children; Refractive Error; Coverage; Nigeria; Eye Health; Vision Impairment
Key messages: In some developing countries even as the need for refractive error services may be low the coverage for the servces is still very low. Also, there other indicators that can complement effective refractive error coverages in assessing refractive error coverage in children.
Introduction
Despite the significance of good sight to childhood development, access to eye health is poor among children in many resource-poor settings. School-age children with vision impairment can experience lower levels of educational achievement and self-esteem than their sighted peers [1]. Vision loss tends to worsen existing gender inequalities in school attendance, with girls more likely to miss school than boys due to vision impairments [2].
The Katsina State Ministry of Health in collaboration with the Noor Dubai Foundation is implementing school eye health. The programme aims to improve the quality of life, socioeconomic status and educational potential of students and teachers of elementary schools. For sustainability of the programme and in consideration of limited resources, the programme targets students in classes one and six only, as recommended by an International agency for prevention of blindness school eye health expert committee report [3].
The programme intends to provide eye screening to 160,000 elementary school children and 3,000 teachers in the state, and provision of spectacles.
One of the targets of the programme is to increase the effective refractive error coverage (eREC) among students by at least 40%, as recommended by the WHA resolution of 73.6, and the United Nations resolution 75th of 2021 on Accelerating SDGS through eye care services [4,5].
A study was conducted with the main objectives of determining the prevalence and types of refractive error among students in classes one and six elementary schools in Katsina State of Nigeria and how it varies among the classes; determine the baseline effective refractive error coverage (eREC), the effective clinical refractive error coverages (eCREC) and the Glasses ‘Need’ among these students and how it varies among the classes. The result of the study will provide baseline data for planning and monitoring of the school eye health programme. This paper reports the findings of this study.
Material and Methods
Study Design
The study was a cross-sectional survey of elementary school students in the three largest cities of Katsina State. The study participants were selected by a two-stage cluster random sampling technique. The data collection took place between April and Oct 2023.
Minimum Sample Size
A minimum sample of 2200 was calculated using the following formula from OpenEpi, Version 3, open source calculator—SSPropor: Sample size n = [DEFF*Np (1-p)]/[(d2/Z21-α/2*(N-1)+p*(1-p)] and the below parameters: [6]
Population size (N): 256,500 students
Hypothesized % frequency of outcome factor in the population (p): 2% [7.8] +/-0.75
Confidence limits as % of 100 (absolute +/- %) (d): 0.75%
Design effect (for cluster surveys-DEFF): 1.5
Confidence interval at 95%
Nonresponse rate of 5%
The average size of a class in the target schools is 40-60 students. We therefore estimated that the minimum sample size will be obtained in 40 classes. In the first sampling stage, 20 schools from a list of all 194 public primary schools in the three cities were randomly selected by probability proportional to size. The second sampling stage involved using simple balloting to randomly select one class each among the class one and class six arms in the school. All students in each selected class were included in the study.
Training of the Research Team
Two-day training was conducted to standardize the procedures for visual acuity testing and eye examination among the ophthalmic nurses using a public health ophthalmologist as the gold standard. The optometrist and optician were also retrained on usage of the auto refractometer equipment. Agreements (kappa coefficient of 0.8) were obtained between the gold standard and the survey team during the training.
Data Collection Procedure
All the selected students had uncorrected visual acuity testing in each eye by the ophthalmic nurse. Those with glasses had their vision retested with their glasses on. Students presenting vision less than 6/12 (with or without spectacles) in any eye had pinhole vision tested for each eye. Visual acuity was tested outdoors using the tumbling E-chart at six meters. The students scored the lowest visual acuity line that they could correctly identify the orientation of four out of the five E-letters. If the pinhole vision in any eye was worse than 6/12, the eye was examined to determine the cause of vision loss. All possible causes were recorded.
A noncycloplegic autorefraction was then conducted using a Topcon KR1 autorefractometer (Topcon, Tokyo-Japan) by the optometrist. Three consecutive readings of the autorefractometer were taken to obtain the average reading.
All those with improved vision after pinhole were referred for refraction, while those with pinhole vision worse than 6/12 were referred to the ophthalmologists for further assessment. Children with mild infective or allergic conjunctivitis were treated with medications. Data were cross-checked daily by the optometrist for any missing data.
Definition of Blindness and Vision Impairment (VI)
Definitions of blindness and VI followed the WHO classification: [9] (1) normal = presenting visual acuity (PVA) ≥6/12 in the better eye; (2) mild VI = PVA <6/12 but ≥6/18 in the better eye; (3) moderate VI = PVA <6/18 but ≥6/60 in the better eye; (4) severe VI = PVA <6/60 but ≥3/60 in the better eye; (5) blindness = PVA <3/60 in the better eye
Definition of Refractive Errors (RE)
Spherical equivalent (SE) was calculated as spherical power plus half of cylindrical power. Only the worse eye with the greater absolute value of SE was used to define RE.
Definition of Refractive Error Coverage
- Emmetropia was defined as SE between -0.5 and +0.50 D.
- Hypermetropia was defined as SE of 2.0 D or higher
- Myopia was defined as SE of less than -0.50 dioptres (D). An SE of less than -5.00 D was considered high myopia.
- Astigmatism was defined as a cylinder power of > 1.00 D or greater.
- Anisometropia was defined as an interocular difference of 1.0 D or more in the SE.
Effective refractive error coverage (eREC) for distance vision for a person was computed by met need/(met need + unmet need + undermet need) × 100%.
- Met need = participants who were using glasses and had uncorrected distance vision of worse than 6/12 in the better eye but presenting vision of 6/12 or better with glasses in the better eye.
- Undermet need = participants with uncorrected vision of worse than 6/12 and presenting vision of worse than 6/12 with glasses but with pinhole vision of6/12 or better.
- Unmet need = participants who were not using glasses and had uncorrected vision of worse than 6/12 in the better eye but pinhole vision of 6/12 or better in the better eye.
Effective refractive error coverage (eREC) for eyes for distance vision was computed by met need/(met need for eyes + unmet need for eyes+ undermet need for eyes) × 100%.
Met need for eyes = number of eyes with uncorrected distance vision of worse than 6/12 in the eye but vision of 6/12 or better with glasses in the eye.
Undermet need for eyes = number of eyes with uncorrected vision of worse than 6/12 and presenting vision of worse than 6/12 with glasses but with pin hole vision of 6/12 or better in the eyes.
Unmet need for eyes = number of eyes without glasses and had uncorrected vision of worse than 6/12 in the eye but pin hole vision of 6/12 or better in the eye.
Effective clinical refractive error coverage (e-CREC) for distance vision was computed by clinical met need/(clinical met need + clinical unmet need + clinical undermet need) × 100%.
Data Analysis
- Clinical met need = students who are using glasses and their vision in any eye cannot be improved to two lines of Snellen’s or more with pinhole but whose uncorrected vision in any eye decreases by two lines of Snellen's chart
- Clinical undermet need = students using glasses but their vision can be improved using a pinhole by at least two lines of Snellen visual acuity chart in any eye.
- Clinical unmet need = students who are not using glasses and their vision can be improved by at least two lines of Snellen with pinhole in any eye.
- Effective Glasses Need is defined as % of students whose presenting vision in any eye can be improved by two or more Snellen’s lines using pinhole.
Data were collected in a questionnaire which was specifically designed for this study (data collection sheet attached as a supplementary file) and entered into a data screen developed using Epi-Data version 3. The few students with missing refractive error data were excluded from the refractive error-related analysis. Double data entry was performed to correct entry error. Data were exported into SPSS version 22 and cleaned. Data analysis was performed using the same SPSS software. Descriptive data are presented in Tables. Comparisons between groups with variables of concern were basically in proportions/percentages with a significance level of p values less than 0.05. Multivariate logistic regression was also used to determine associated factors (age groups, sex, class) for selected refractive error categories (myopia, hypermetropia and astigmatism). Odds ratios, confidence intervals and p values were determined. Significant differences between odd ratios were determined by p values of less than 0.05.
Results
A total of 2335 students were enumerated, of which 2224 students were examined, for a response rate of 95.2%. Eleven students (0.5%) were absent from the school during the study. Class one students constituted 49.9% (1110) of the examined students. The mean age for class one students was 6.9 years (SD 1.4), with an age range of 5-13 years, while for class six students, the mean age was 12 years (SD 1.3), with a range between 10-16 years. Boys were 49.9% and 50.8% of the students in classes one and six, respectively, as shown in Table 1.
Prevalence of Blindness and Vision Impairment
Among class six students, one student was blind (0.04%), seven had moderate vision impairment (VI) (0.6%) and four had mild VI (0.4%). For class one students, no child was blind, but two children each had severe (0.2%) and moderate VI (0.2%). Major causes of blindness and vision impairment were nystagmus, cataracts, microphthalmos, and corneal scarring (Table 2).
Refractive Errors
As shown in Table 2, class six students, had higher prevalence of myopia (20.1% vs 10.9%, p < 0.001), and Astigmatism (11.1% vs 7.9%, p 0.01) than class one students. They also have higher prevalence of hypermetropia but it is not statistically significant (2.0% vs 1.1%, p 0.08). Anisometropia was detected in a total of 40 students more among the class six students (2.3% vs 1.4%, p 0.11) though the difference is not statistically significant.
Class six students had higher odds of Myopia (OR 2.05 [1.62 – 2.60] p <0.001) and astigmatism (1.44 [1.08 – 1.92]) p 0.012) than class one students. Although the Class six students had higher odds ratio of hypermetropia (1.85 [0.91 to 3.75]); p 0.085) it is not statistically significant.
Males have higher risk of myopia than females (OR 1.34 [1.04-1.64]), but there was no difference in gender across other categories of refractive error.
Higher age groups (11-15 years) had higher odds of myopia (1.82 [0.91- 3.75] p<0.001). Age groups does not seem to be a risk factor for hypermetropia. Table 3.
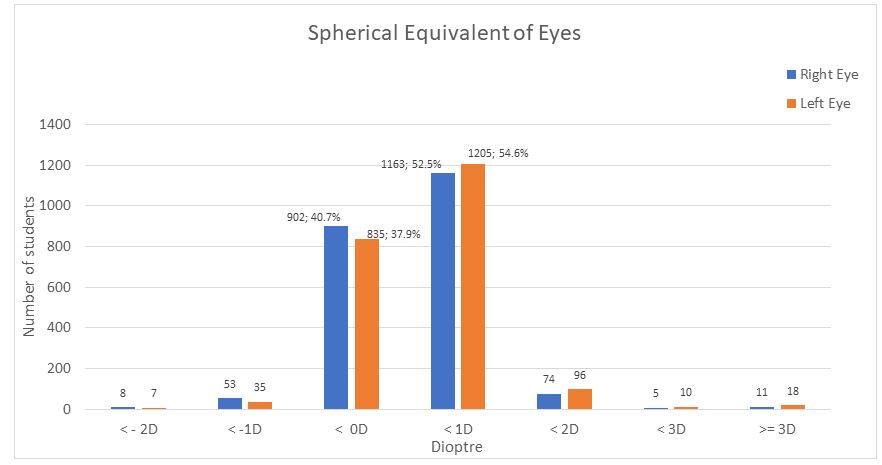
Right eyes had Spherical Equivalent of -1 D to +1 D in 92.9% of the eyes, while it was 91.7% in the left eyes (Figure 1).
Effective Refractive Error Coverage
The eREC (person) was 33.3% for class six students, but for class one students, there was no student using glasses, and there was no student in the ‘unmet need’ category. The eREC (eyes) was 22.2% for class six, but for class one, it was 0%, with only one eye as the unmet need. The eCREC was 10% for class six but 0% for class one as there was no ‘met need’. Table 4. The effective Glasses ‘need’ was 0.9% and 0.2% for classes six and one respectively. Table 4.
Discussion
This study reports the prevalence of different categories of refractive error among two class groups (class one and class six) of elementary school children and the effective refractive error coverage in the class groups.
The study identified myopia to be more common among older school children (ages 11-16 years) in class six (20.1%) than among younger children (ages 5-7 years) in class one, which had a prevalence of 10.9%. The study further reported low prevalence of hypermetropia with the prevalence higher among the class six students (2.0% vs 1.1%, p 0.08) although the difference was not statistically significant. In Ireland, a study among similar age groups reported myopia prevalence of 19.9% among 12- to 13-year-old children and 10.9% among 5- to 7-year-old children, while hypermetropia was 8.9% among older children and 25% among younger age groups [10]. Similarly, a study in Chile also reported 26.3% hypermetropia for younger children and myopia of 19.4% among older children [11]. A study in Xianjian province of China reported a myopia prevalence of 13-27% among school children across different ethnic groups [12].
A systematic review of myopia among children in Africa reported an overall prevalence of 4.7% among all age groups (95% CI 3.3-6.5%) and 5.8% among 12-18 years, with a projection of 17.4% by 2050 in an urban setting [13]. A Nigerian hospital-based study in the city of Ibadan reported myopia prevalence of 23.2% and hypermetropia prevalence of 16.5% among 11-15-year-olds [14]. However, another South‒east Nigerian study reported a very low prevalence of refractive error among children, with myopia prevalence of only 1.9% and hypermetropia prevalence of only 0.1% among school-age children [15]. However, this study only assessed the refractive status of children with vision of less than 6/9. Thus, the study might have missed many children who could have some mild refractive error but normal vision. Generally, our study’s higher prevalence figures for myopia and lower prevalence of hypermetropia may be related to the noncycloplegic refractive error data we used, which would overestimate the myopia and underestimate hypermetropia especially the mild ones. It has been reported that cycloplegic refractive error readings are often 30% lower than noncycloplegic readings for myopia [13]. Our study had to be conducted with non-dilated recordings of refractive errors because the Ministry of health ethical committees denied approval for use of dilating drops on the students during the study unless some stringent measures are met
The study found that the eREC among children in class six is 33%. There are very limited studies to compare with our data, as most eREC studies are on adults. The available school children studies mostly measured spectacle coverage, not effective refractive error coverage, as the concept of the eREC is relatively new. This point was highlighted by a recent Lancet publication that reviewed global data on eREC. It called for the generation of more data on eREC among children [16].
In the urban Indian city of New Delhi, the spectacle coverage among the children was 29.3% (27.1-31.7%) [17]. A Chilean study in two urban centers found spectacle coverage for children to be in the range of 8.2-10.8% [18]. In the Xianjing province of China, which has higher levels of myopia, the spectacle coverage was up to 36% [19].
The eREC is one of the adopted indicators for universal health coverage and is a component of UN sustainable development goal (SDG) number three (health and wellbeing) [5]. The eREC measurement should ideally cover both adult and children refractive error services since refractive error is also quite common among children, and the projected global epidemic of myopia, mostly among children, is on the horizon [20]. However, the current available eREC data are mainly from the adult population. This fact has been alluded to by the recent global review on eREC, which presented no data on eREC among children [16]. For the comprehensive monitoring of eREC and attainment of Universal Health Coverage (UHC) data, the refractive error services indicator among children must be generated and monitored. Furthermore, current reporting of eREC is based on eREC for persons. However, it is also useful for local assessment and monitoring of refractive error services to consider the eREC for eyes, as it gives more detailed individual-level refractive error coverage, and it is often lower than the eREC for persons, as shown in this study with eREC for persons as 33% vs 10% for eREC for eyes.
Although the eREC readily identifies crude coverage of refractive services, in practical terms, it is the eCREC as defined in this study that would show the need or attainment of coverage for refractive error services. This indicator relates more to routine clinical practices for the optical correction of refractive errors. In clinical practice, optical correction is not limited only to corrections that reach 6/12 vision. Any significant vision improvement (possibly any two lines of visual acuity improvement) with glasses is amenable to treatment. In our study, even though the eREC for older children was 33%, the eCREC was only 10%, showing a wide difference between the two indicators. We feel the latter may be a more practical measure for monitoring and planning optical services or at least the two indicators should be reported together. We could not get any study that has reported the concept of eCREC as mentioned here, so as to compare with.
Limitations
Our study did not collect cycloplegic refraction data because of the stricter ethical approval requirements from the local health authorities this must have overestimated the myopia while underestimating the hypermetropia. Sampling only pupils in classes one and six for the study may have exaggerated the prevalence of refractive error in the study as children in the age brackets in these classes often have higher refractive errors than children in the other classes. Additionally, the few numbers of ‘met need’, ‘undermet need’ and ‘met need’ means that the percentage calculations may not be reliable. This may have affected our results and limited comparison of our data with some other studies. However, the results are still useful baseline data.
Conclusion
The prevalence of refractive error among primary school students in Katsina state is comparatively similar to other studies using the same methodology (noncycloplegic refraction). The eREC is low in the state even as the need for refractive error services seems low. In addition to eREC as a main indicator to monitor refractive error services, other useful indicators may be eCREC and effective glasses need.
Source(s) of support
Noor Dubai Foundation, UAE
Conflicting Interest
None
Authors' contributions
Muhammad Mansur Rabiu: Developed the study conception, study design, executed the field work, acquisition of data, data analysis and interpretation, drafted the article and revised it after inputs from other authors.
Manal O Taryam: Study design, fund acquisition, data interpretation, written part of the article, revised the whole article.
Nasiru Muhammed: Reviewed the study design and data interpretation, drafted a portion of the article and substantially revised the article.
Ahmed A Abubakar: Data entry, data analysis, drafting parts of the article and revision of the whole article.
Abduljalil U Abdullah: Literature review, data acquisition, drafting parts of article, and revision of whole article.
Fatima Kyari: Manuscript drafting and review.
Acknowledgments
We wish to thank the Katsina State Ministry of Health and the State Basic Education Board for approving the conduct of the study. We also appreciate the field team members consisting of nurses and optometrists who collected the data. Finally, we express gratitude to the teachers and parents who consented to the participation of their wards in the study.
Ethical Approval and Informed Consent
All methods were carried out in accordance with relevant guidelines and regulations and performed in accordance with the Helsinki Declaration. All experimental protocols were approved by the Ethical medical committee of the Ministry of Health Katsina, Nigeria with the following Ethical approval reference (MOH/ADM/SUB//1152/1//566).
Informed consent from the parents/school teachers of each selected student was sought in writing before including them in the study.
Data Availability
The data of this study are present in the computer of the corresponding author at the Noor Dubai Foundation Africa office, Katsina, Nigeria.
- World report on vision, Geneva: World Health Organization, Geneva (2019) Available at https://www.who.in t/publications/i/item/9789241516570. Accessed on 13 November 2022.
- Education info sheet, available at https://www.sight savers.org/disability/education/ Accessed on 3 January 2022.
- Standard school eye health guidelines for low and middle-income countries, p. 13, International Agency for the Prevention of Blindness (2018) available at https:/www.iapb.org /wp-content/uploads/Guidelines-School-EyeHealth-Programmemes-English-Final.pdf
- World Health Organization. 74th World Health Assembly A74/9 Add.3. Integrated people-centered eye care, including preventable vision impairment and blindness. Global targets for 2030 Available at https://apps.who.int/gb/eb wha/pdf_files/WHA74/A74_9Add3-en.pdf. Accessed 23 December, 2021
- United Nations General Assembly. 75th session. Agenda item 24. Eradication of poverty and other development issues. Vision for Everyone: accelerating action to achieve the Sustainable Development Goals. A/RES/75/310. Available at https://undocs.org/en/A/RES/75/310. Accessed on 23 December 2021.
- http://www.openepi.com/SampleSize/SSPropor.htm. accessed on January 15, 2022
- Ajaiyeoba AI, Isawumi MA, Adeoye AO, Oluleye TS (2005) Prevalence and causes of blindness and visual impairment among school children in southwestern Nigeria. Int Ophthalmol. 26: 121-5.
- Opubiri I, Pedro-Egbe C (2013) Screening for refractive error among primary school children in Bayelsa State, Nigeria. Pan Afr Med J. 14: 74.
- WHO ICD 11 classification of VI (9D90) https://icd.who.int/browse11/l-m/en#/http%3a%2f%2fid.who.int%2ficd%2fentity%2f1103667651. Accessed on 12/03/2022.
- Harrington SC, Stack J, Saunders K, O'Dwyer V (2019) Refractive error and visual impairment in Ireland schoolchildren. Br J Ophthalmol. 103: 1112-8.
- Maul E, Barroso S, Munoz SR, Sperduto RD, Ellwein LB (2000) Refractive Error Study in Children: results from La Florida, Chile. Am J Ophthalmol. 129: 445-54.
- Chin MP, Siong KH, Chan KH, Do CW, Chan HH, Cheong AM (2015) Prevalence of visual impairment and refractive errors among different ethnic groups in schoolchildren in Turpan, China. Ophthalmic Physiol Opt. 35: 263-70.
- Kobia-Acquah E, Flitcroft DI, Akowuah PK, Lingham G, Loughman J (2022) Regional variations and temporal trends of childhood myopia prevalence in Africa: A systematic review and meta-analysis. Ophthalmic Physiol Opt. 42: 1232-52.
- Olusanya BA, Ugalahi MO, Ogunleye OT, Baiyeroju AM (2019) Refractive errors among children attending a tertiary eye facility in Ibadan, Nigeria: highlighting the need for school eye health programmes. Annals of Ibadan postgraduate medicine, 17: 49-59.
- Maduka-Okafor FC, Okoye O, Ezegwui I, et al. (2021) Refractive Error and Visual Impairment Among School Children: Result of a South-Eastern Nigerian Regional Survey. Clin Ophthalmol. 15: 2345-53.
- Bourne RRA, Cicinelli MV, Sedighi T, Tapply IH, McCormick I, et al. (2022) Vision Loss Expert Group of the Global Burden of Disease Study; RAAB International Co-Author Group. Effective refractive error coverage in adults aged 50 years and older: estimates from population-based surveys in 61 countries. Lancet Glob Health. 11: S2214-109X(22) 00433-8.
- Gupta V, Saxena R, Vashist P, Bhardwaj A, Pandey RM, Tandon R, Menon V (2019) Spectacle Coverage among Urban Schoolchildren with Refractive Error Provided Subsidized Spectacles in North India. Optom Vis Sci. 96: 301-8.
- Barria F, Conte F, Muñoz S, Leasher JL, Silva JC (2018) Prevalence of refractive error and spectacle coverage in schoolchildren in two urban areas of Chile. Rev Panam Salud Publica. 42: e61.
- Chin MP, Siong KH, Chan KH, Do CW, Chan HH, Cheong AM (2015) Prevalence of visual impairment and refractive errors among different ethnic groups in schoolchildren in Turpan, China. Ophthalmic Physiol Opt. 35: 263-70.
- Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, et al. (2016) Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology. 123: 1036-42.

Tables at a glance
Figures at a glance