Figure 1 Kaplan Meier survival function by baseline ART regimen
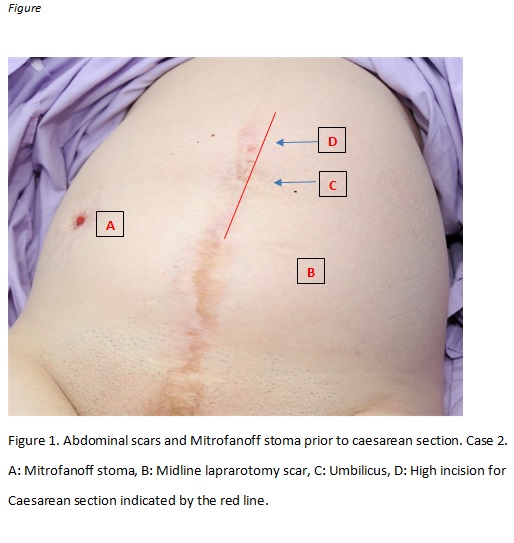
Figure 1 Kaplan Meier survival function by baseline ART regimen
|
Congenital anomaly |
Perinatal complications |
Delivery method |
Outcome |
Case 1 |
Bladder exstrophy |
Miscarriage X1 |
Emergency Classical caesarean section due to preterm labour |
Nil significant maternal complications |
Case 2a |
Bladder exstrophy |
Miscarriage X1 (twins) |
Elective caesarean section |
Maternal: small bowel injury |
Case 2b |
2nd pregnancy for case 2 |
Recurrent UTIs |
Elective caesarean section |
Maternal: minor bladder serosal tear |
Case 3a |
Cloacal exstrophy |
Miscarriage X1 |
Elective caesarean section |
Nil significant complications |
Case 3b |
2nd pregnancy for case 3 |
Recurrent UTIs |
Emergency caesarean section |
Maternal: Indwelling catheter pushed through a fold into vagina |
Table2 Summary of the cases
Study (Arthors) |
Year |
Number of women |
Number of pregnancies |
Outcomes |
Gestation at delivery |
Mode of delivery |
Ref |
Dy et al. |
2015 |
12 |
22 |
Live birth 14 (64%), Terminations 4(18%), Spontaneous abortion <24 weeks 4(18%). |
Mean gestational age at delivery: 36 weeks |
Caesarean section in all 14 cases |
22 |
Deans et al. |
2012 |
52 |
57 |
Live birth 34 (56%), Miscarriage 21 (35%), Termination 1 (2%), Stillbirth 4 (7%) |
Median gestational age of all live births was 37 weeks. |
All patients deliered by cesarean section of which 3 were emergencies. 3 classical cesarean sections. |
18 |
Ebert et al. |
2011 |
2 |
3 |
Live birth 2 (67%); Miscarriage 1 (33%) |
one at 39 weeks, one at 33 weeks |
1 by elective LUSCS, 1 by emergency LUSCS at 33+4/40 due to preterm labour |
19 |
Rubenwolf et al. |
2016 |
12 |
17 |
Live birth 16 (94%); Miscarriage 1(6%) |
Not mentioned |
All delivered by elective caesarean section |
24 |
Eswara et al. |
2016 |
|
|
|
Mean gestational age at delivery: 36 weeks |
|
23 |
Schumacher et al. |
1997 |
6 |
7 |
Live birth 7(100%) |
Not mentioned |
All delivered by caesarean section |
12 |
Mathews et al. |
2003 |
6 |
11 |
Live birth 7 (63%), Miscarriage 2(18%), TOP 2 (18%) |
Not mentioned |
6 by caesarean section, 1 had uneventful vaginal birth |
11 |
Gezer et al. |
2011 |
1 |
1 |
Live birth 1 (100%) |
36 weeks |
Emergency Classical C/Section due to preterm labour |
20 |
Giron et al |
2011 |
14 |
22 |
Healthy babies 17 (77.2%); Miscarriage 4 (18.1%); Neonatal death 1 (4.7%) |
Not mentioned |
All babies were delivered through caesarean section ith the exception of one that had a premature normal birth |
9 |
Bildirin et al. |
2012 |
1 |
1 |
Live birth 1 (100%) |
34 |
Vaginal birth |
16 |
Greenwell et al. |
2003 |
20 |
37 |
Live birth 29 (78%), Miscarriage 6 (16%), TOP 2 (5%) |
Mean gestational age at delivery: 36.9 weeks (35-40) |
Elective Caesarean section 13 (43%), Emergency Caesarean 7 (23%); vaginal birth 10 (34%) |
10 |
Burbigi et al |
1986 |
5 |
7 |
Live birth 6 (86%), 1 TOP (14%) |
Not mentioned |
3 caesarean sections (50%); 3 vaginal birth (50%) |
17 |
Mantel et al. |
2000 |
3 |
6 |
Live birth 2 (33%), Miscarriage 4 (66%) |
35 and 36 weeks |
Emergency Caesarean sections for malpresentation in labour (100%) |
1 |
Table1 Literature summary of the pregnancy outcomes of the women with congenital bladder exstrophy or cloacal exstrophy
Perinatal issues |
Perinatal management |
High risk for multiple complications |
Pregnancy to be considered high risk, collaborative approach between an experienced obstetrician with skills in paediatric and adolescent gynaecology and a urologist with experience in congenital anomaly reconstructive surgery for antenatal care and delivery planning |
Fertility issues(1) |
Aware and management as per conventional treatment for sub fertility |
1:70 risk of congenital bladder exstrophy in the fetus which is a 500 fold increase over the general population(2) |
Prenatal USS for detection |
Urinary tract obstruction; Hydronephrosis |
USS of the renal tract, first at 16 weeks, thereafter Q6-8 weeks, stenting or nephrostomy if obstructed;(3) recommend percutaneous drainage of the kidneys for the following indications: pain, progressive hydronephrosis, rising serum creatinine, febrile UTIs, recommend not removing the nephrostomy tubes until 1 week postpartum. Biggest risk period for obstruction appears to occur between 20 and 28 weeks of gestation, patient at risk may require USS every 2 weeks during that time(4) |
Urinary tract infections |
Baseline renal function and urine microscopy; screening for asymptomatic bacteriuria weekly; adequate hydration; proactively completely empty bladder at regular intervals advised; prophylactic antibiotics if recurrent UTIs, treat only febrile UTIs (3) |
Stomal prolapse or parastomal hernia |
Typically resolve after delivery |
Worsening renal function, development of end stage renal failure (4) |
Close monitoring, regular renal consultation. |
Catherisation difficulties |
Indwelling catheter or change the type and length of the catheter used (e.g. Coude tip catheter)(4) |
Cervical incompetence |
Monitor cervical length |
Preterm labour |
Having a planned delivery at late preterm gestations after steroid cover |
Miscarriage |
Early USS to confirm gestation, identify anomalies |
Malpresentation |
Planned delivery, aware of the presentation at the time of the delivery |
Renal stone |
Adequate hydration, proactively completely empty bladder at regular intervals, if suspicious of renal stone, USS and urology management |
Urinary incontinence |
Generally recover to pre-pregnancy status postpartum |
Uterine prolapse including cervical prolapse |
Cervical pessary, a diaphragm fitting ring, bed rest for late gestation(5) |
Hypertensive disorders |
Monitoring of the blood pressure and blood biochemistry and urine protein |
Low lying placenta with antepartum haemorrhage |
USS for detection, management according to standard low lying placenta management protocol |
Delivery |
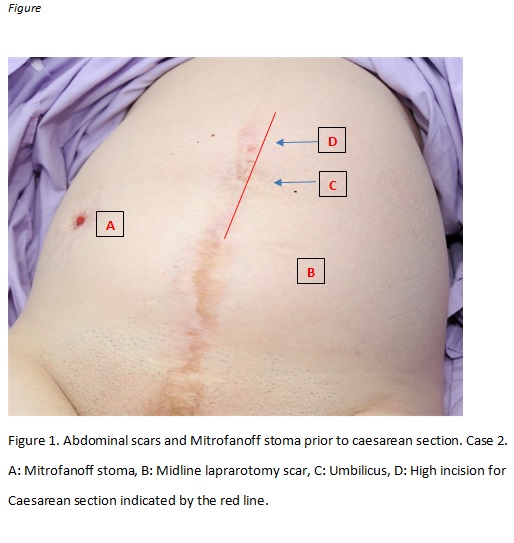
Elective Caesarean section in the exstrophy population was the clear consensus.(4) Planned caesarean section at late preterm gestations after steroid cover; Surgery to be done by experienced obstetrician with urologist in theatre, with suitable neonatology service on site; High midline abdominal skin and wall incision, lower segment uterine incision or classical uterine incision pending on status of adhesion. Vaginal birth only is considered in uncomplicated pregnancies.(6) |
Table3 Summary of recommendations of pregnancy management and delivery)