A Rare Non-Functional Bladder Paraganglioma Managed by Transurethral Resection
Received Date: September 23, 2021 Accepted Date: October 23, 2021 Published Date: January 10 ,2022
doi: 10.17303/jurh.2022.1.101
Citation: Maatougui Jasser (2021) A Rare Non-Functional Bladder Paraganglioma Managed by Transurethral Resection. J Urol Renal Health 1: 1-7.
Abstract
Background: Paraganglioma of the urinary bladder is rarely encountered. Its clinical signs and symptoms are usually nonspecific.
Case Presentation: We report a case of a 48-year-old woman who presented with recurrent hematuria for last 2 months with a recently detected hypertension. Computed tomography (CT) revealed a lobulated mass arising from the posterior wall of the urinary bladder and protruding into the vesical lumen measuring 3cm with inhomogeneous postcontrast enhancement. Transurethral resection of the mass has instantly produced a hypertensive peak (200/110 mmHg) leading to an interruption of operation. Pathology of the specimen found a pheochromocytoma. Our patient denied a history of dizziness, sweating, and palpitations during micturition. Hormonal evaluation showed a normal level of both plasmatic and urinary metanephrine and normetanephrine. Metastatic workup was negative. Both adrenal glands were normal at CT. MIBG scan showed an increased localized activity in the bladder. After preoperative stabilization of hypertension and medical preparation, a complete transurethral resection of the tumor was performed. This case was discussed at a tumor board meeting and surveillance was decided. The patient has been disease-free for 9 months.
Conclusion: In patients with unusual, striking symptoms and an increase in blood pressure with micturition, diagnosis of pheochromocytoma of the urinary bladder must be considered. Imaging will help in confirming the diagnosis and localizing the tumor. Surgical removal is the treatment of choice.
Keywords: Pheochromocytoma; Bladder
Introduction
Paraganglioma of the urinary bladder (PUB) rarely encoutered. Pheochromocytoma that arise outside the adrenal gland is called paraganglioma [1]. It is a neuroendocrine neoplasm arising from chromaffin cells located in the muscle of the bladder wall muscle [2]. Its clinical expression is paroxysmal associating sweating, headache and tachycardia [3]. It can be non-functional or functional by hormonal screening. Establishing the diagnosis may be difficult. Histological examination is often the only key leading to diagnosis [2]. Its treatment is surgical.
We report the clinical features and pathological characteristics of a patient diagnosed as paraganglioma of the urinary bladder managed by monobloc transurethral resection.
Case Presentation
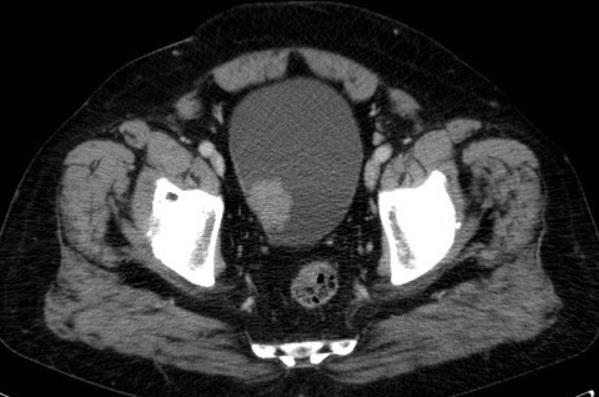
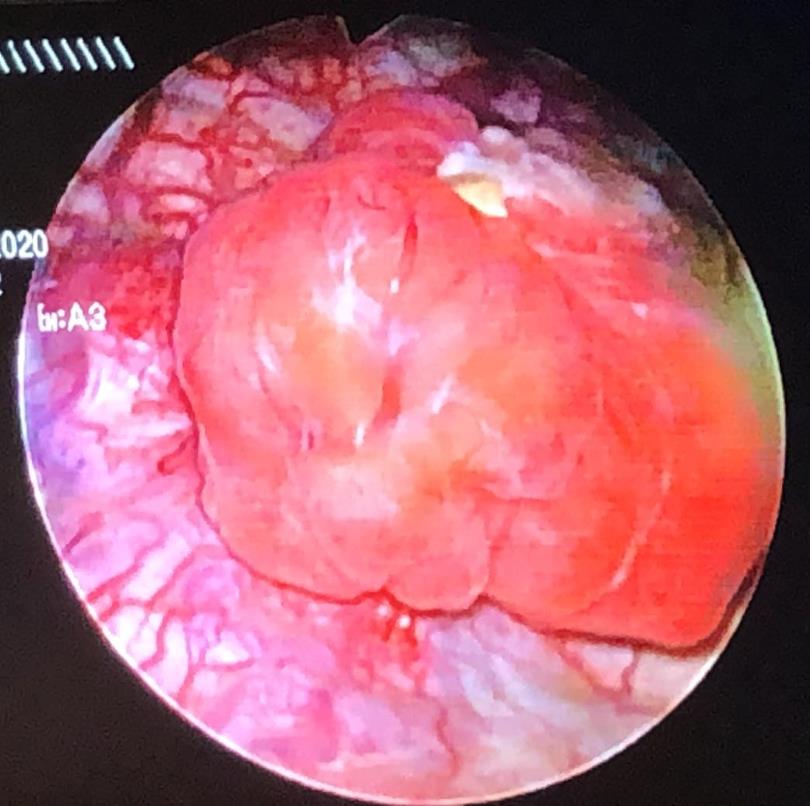
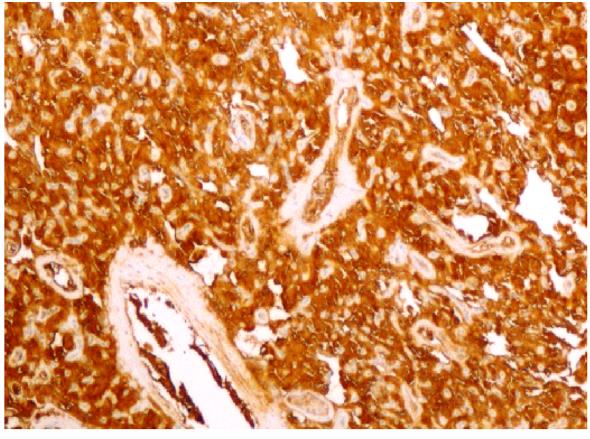
We report a case of a 48-year-old woman who presented with recurrent hematuria for last 2 months with a recently detected hypertension. Computed tomography (CT) revealed a mass arising from the posterior wall of the urinary bladder measuring 3cm with inhomogeneous contrast enhancement (Figure 1). Cystoscopy showed a mass covered by smooth vesical mucosa, (Figure 2). Transurethral resection of the mass has instantly produced a hypertensive peak (200/110 mmHg) leading to an interruption of operation. Pathology of the specimen has confirmed the diagnosis of a bladder paraganglioma (Figure 3).
Our patient denied a history of dizziness, sweating, and palpitations during micturition. Hormonal evaluation showed normal levels of plasmatic and urinary metanephrine and normetanephrine (VMA, HVA). Metastatic workup was negative. Adrenal glands were normal at CT. MIBG scan showed an increased isolated activity in the bladder. After preoperative stabilization of hypertension and medical preparation using alpha-blockers, a complete transurethral resection of the tumor has been performed (Figure 4).
The patient was discharged two days after the operation without any postoperative complications. This case was discussed at a tumor board meeting and surveillance was decided. The patient has been disease-free for 9 months.
During the postoperative follow-up, our patient was completely asymptomatic. It presented no more hematuria and neither high blood pressure. Post-operative MIBG was normal as well as the metanephrines.
Discussion
Extra-adrenal localization of pheochromocytoma is rarely encoutered [1,4], it is found in 10–15% of cases [5]. The first case with a bladder localization was described by Zimmerman in 1953 [6]. In the literature, fewer than 200 cases that has been described [7].
The average age of predilection is 40 years with extremes ranging from 10 to 74 years [1]. Women are more concerned then men [8]. Functional paragangliomas secrete catecholamines, which may lead to symptoms such as palpitations, dizziness, and sweating. These symptoms are mainly precipitated by micturition or overdistention of the bladder, defecation, sexual activity or any bladder instrumentation such ass cystoscopy or transurethral resection [8,9].
Imaging findings are indistinguishable from other tumor types. The Meta-iodo-benzyl-guanidine (MIBG) scan is regarded as high specific for paraganglioma. However, its use is limited because of its expense and restricted availability [10]. In our patient, MIBG scan showed an increased localized activity in the bladder with no other localisations.
In some cases, such as in our case, urinary catecholamine levels may be normal if the tumors are small at the time of diagnosis and because catecholamine secretion may increase for only brief periods during contraction of a distended urinary bladder [11].
In our case, if the PUB was suspected when transurethral resection of the mass has instantly produced a hypertensive peak (200/110 mmHg). Metanephrines levels were normal, metastatic workup was negative and both adrenal glands were normal.
There is no standard treatment for PUB. The benefit of chemotherapy and radiotherapy is not well established [3]. Surgical removal is the treatment of choice [3]. Various surgical options are available including transurethral resection, partial cystectomy and radical cystectomy. Some specialists indicated that partial cystectomy is the mainstream treatment [12]. To avoid hypertensive spikes during the mass manipulation, preoperative treatment with alpha-blockers is required, started 1 to 3 weeks before surgery [13]. Katiyar et al. [14] reported two non-functional PUB patients who underwent transurethral bladder resection tumor in which no recurrence after follow-up for 6 and 10 months, indicating that TURBT is an effective treatment for non-functional PUB. In contrast, it has been suggested that resection rarely excises all the tumor as the neoplasms often invade the submucosa and muscularis of the urinary bladder leading to potential tumor recurrence [15].
We successfully treated our patient with a trans-uretral resection. No recurrence or metastasis were found at 9-months follow-up. Therefore, the complete resection of the tumors through the transurethral approach seems to be a curative option and may represent the mainstream future treatment [14].
In general, PUB is a rare tumor with a good prognosis and slow development [15]. However, paraganglioma has a tendency for recurrence and metastasis.
Conclusion
In patients with unusual, striking symptoms and an increase in blood pressure with micturition, diagnosis of paraganglioma of the urinary bladder must be considered. Imaging will help in confirming the diagnosis and localizing the tumor. Surgical removal is the treatment of choice. Complete transurethral resection is a safe and efficient treatment that serves both diagnostic and therapeutic purposes. Long-term follow-up is recommended.
- Grignon DJ (1997) Urologic Surgical Pathology. St Loius: Mosby; 1997. Neoplasm of the urinary bladder 1997: 215-305.
- Siatelis A, Konstantinidis C, Volanis D (2008) Pheochromocytoma of the urinary bladder: report of 2 cases and review of literature. Italian J Urol Nephrol 60: 137–40.
- Jandou I, Moataz A, Mouqtassid MH (2020) The ectopic vesical pheochromocytoma a diagnostic and therapeutic challenge case report and literature review. Int J Surg Case Rep 77: 857-61
- Jandou I, Moataz A, Mouqtassid MH (2020) The ectopic vesical pheochromocytoma a diagnostic and therapeutic challenge case report and literature review. Int J Surg Case Rep 77: 857-61.
- JH Alexandre, JP Fraioli, JC Boucherie (1983) Phéochromocytomes : diagnostic, anesthésie et traitement. A propos de 17 observations récentes, Ann. Chir 37: 263–71.
- Zimmerman IJ, Biron RE, Macmahon HE (1953) Pheochromocytoma of the urinary bladder. N Engl J Med 249: 25-6.
- Glenn F, Gray GF (1976) Functional tumors of the organ of Zuckerkandl. Ann Surg 183: 578-86.
- Jandou I, Moataz A, Mouqtassid MH, Dakir M, Debbagh A, Aboutaieb R (2020) The ectopic vesical pheochromocytoma a diagnostic and therapeutic challenge case report and literature review. Int J Surg Case Rep 77: 857-61.
- Cheng L, Leibovich BC, Cheville JC (2000) Paraganglioma of the urinary bladder: can biologic potential be predicted?. Cancer 88: 844-52.
- Whalen RK, Althausen AF, Daniels GH (1992) Extra-adrenal pheochromocytoma. J Urol 147: 1-10.
- Gittes RF, Mahoney EM (1997) Pheochromocytoma. Urol Clin North Am 4: 239-52.
- Beilan JA, Lawton A, Hajdenberg J, Rosser CJ (2013) Pheochromocytoma of the urinary bladder: a systematic review of the contemporary literature. BMC Urol 13: 22.
- Pichler R, Heidegger I, Klinglmair G (2014) Unrecognized paraganglioma of the urinary bladder as a cause for basilar-type migraine. Urol Int 92: 482-7.
- Katiyar R, Dwivedi S, Trivedi S, Patne SC, Dwivedi US (2016) Non-Functional Paraganglioma of the Urinary Bladder Treated by Transurethral Resection: Report of Two Cases J Clin Diagn Res 2016: 10.
- Pahwa HS, Kumar A, Srivastava R, Misra S, Goel MM (2013) Urinary bladder paraganglioma-a case series with proposed treating algorithm based on our experience and review of literature. Indian J Surg Oncol 4: 294-7.


Figures at a glance