Migrated Intrauterine Device in Bladder
Received Date: June 03, 2024 Accepted Date: July 03, 2024 Published Date: July 06, 2024
doi: 10.17303/jwhg.2024.11.104
Citation: Shazia Batool, Muhammad Zahid (2024) Migrated Intrauterine Device in Bladder. J Womens Health Gyn 11: 1-6
Abstract
Intrauterine contraceptive device CU-IUCD is commonly used reversible method of contraception due to its safety n cost effectiveness, but if left without follow-up can cause complications. This report presents a case of CU-IUCD in bladder wall and was managed surgically. A 26-year-old female para 4 all vaginal deliveries presented to us after one year of IUCD placement with lower abdominal pain and hematuria. Patient was normal clinically and microbiologically. On ultrasound and X ray IUCD was found outside uterus and not free floating in bladder also which was removed surgically. As IUCDs are long acting, follow up by trained personnel to feel and locate IUCD thread at least every 6 month must be mandatory and if misplaced IUCD found in bladder wall can be removed by just 0.5 cm incision.
Keywords: Misplaced IUCD; Intravesical IUCD; Intrauterine Contraceptive Device; Obstetrics & Gynecology
Introduction
The intrauterine contraceptive device (IUCD) stands as the most widely used method of reversible contraception globally. The IUCD is small T-shaped instrument used for birth control, being inserted into the uterus for prevention of pregnancy. This is the popular type of long-acting reversible birth control method. Around 14% of women opt for this form of contraception due to its high efficacy, safety, and affordability. There are two main types of IUCDs: the hormonal IUCD, which releases levonorgestrel, and the copper IUCD (TCu 380A), which releases copper ions [1]. Among these, the copper IUCD is the most widely available and is the fourth most popular choice among women of childbearing age in Burkina Faso [2].
The copper IUCDs have aminute failure rate of 0.8% whereas hormonal devices reduce this rate below 0.2% while copper IUCDs have shown their effect till fifth day of unprotected intercourse. Despite its benefits, the IUCD is not without complications [3]. These complications include painful cramps and up heavy menstrual bleeding. Even women with hormonal IUCDs may observe daily spotting for weeks and or months. More serious complications consist of expulsions among 2-5% of women and scarce cases of uterus perforation. One of the significant challenges faced by gynecologists is IUCD migration. Typically, IUCD migration occurs into the abdominal cavity, but there have been cases where it has migrated into the adnexa, iliac vein, and broad ligament. Intravesical migration, where the IUCD migrates into the bladder, is a particularly rare complication [4].
CopperIUCDs are most commonly used contraceptives worldwide.as these are long acting and cost effective and safe during breast feeding, non-hormonal and no systemic side effects. Generally being safe can be associated with irregular menstrual cycle n uterine perforation. Reported risk of uterine perforation is 0.5 to 13/1000 and in 85% cases uterine perforation is asymptomatic [5]. This report aims to present a case of missing copper IUCD which lately found in bladder wall with complications.
Case Report
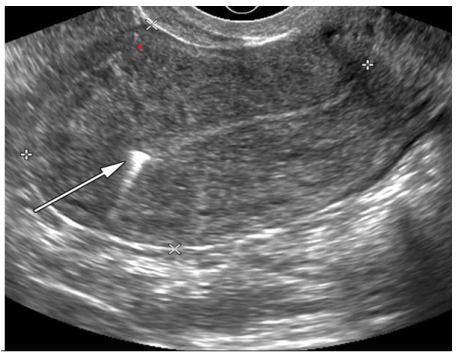
A 26-year-old female para 4 all vaginal deliveries presented to us after one year of IUCD placement with lower abdominal pain and hematuria. The clinical examination conducted on the patient indicated the presence of tenderness in the hypogastric region, along with a moderate degree of inflammation at the urethral meatus. In contrast, the gynecological examination did not reveal any abnormalities and was considered normal. To further investigate the potential cause of these symptoms, urine microscopy and culture tests were performed. The results from these tests did not show any signs of infection, confirming the absence of bacterial or other infectious agents in the urine. On ultrasound and X ray IUCD was found outside uterus and not free floating in bladder also. Surgical removal of IUCD was planned and on opening abdominal wall IUCD thread was found between uterus and bladder coming out from bladder wall. We followed thread to locate IUCD. Once found in bladder wall, IUCD was held firmly with one hand and small 0.5 cm incision made at level of IUCD arm. IUCD was grasped with artery forceps n removed. Bladder wall repaired. Catheter placed in situ for two weeks.
Discussion
The IUCD is widely regarded as the most popular method of reversible contraception in developing countries due to its high efficiency and low cost. However, during pre-insertion counseling, patients are often not informed about rare complications, such as the intravesical migration of the device. This lack of information can lead to medico-legal issues if such complications arise [6]. IUD migration into structures adjacent to the uterus is an uncommon complication, occurring in approximately 1 in 1,000 insertions. The literature primarily consists of case reports and case series on this subject. For instance, Goyal et al. reported only 2 cases of migration, including intravesical migration, out of 240 copper-bearing IUDs inserted over a 12-month period in India [7]. This case represents our first encounter with such a complication in five years of our gynaecological practice.
The insertion of an IUCD is a medical procedure, and preinsertion counseling typically covers common complications such as spotting, heavy periods, pelvic pain, infection, and the possibility of pregnancy. However, the rare complication of IUCD migration is seldom mentioned. IUCD migration usually occurs following partial or complete uterine perforation during insertion. This risk is higher in patients with a scarred myometrium from previous surgeries or with a misdiagnosed hypoplastic, retroverted, or hyperanteverted uterus. Local inflammation caused by the copper IUCD can further facilitate this migration.
Clinically, a migrated IUCD might be discovered incidentally during a routine evaluation without any prior symptoms. Conversely, a patient might present with lower urinary tract symptoms (LUTS), such as urgency, urinary frequency, hematuria, or vaginal discharge. In some cases, a urogenital fistula, such as a vesicouterine fistula, may be the main presenting feature [8]. Bladder stones, a complication of IUCD migration into the bladder, can cause obstructive lower urinary tract symptoms, including straining during urination and acute urinary retention.
Diagnosis often requires imaging and endoscopy. Bladder imaging, such as a full bladder ultrasound, can help identify a foreign body in the bladder, as was the case here. Cystoscopy is essential for a thorough bladder evaluation, determining the presence of foreign bodies like calculi and assessing the extent of migration into the bladder [9]. Tests like the blue methylene test or cystography are useful to rule out fistulas.
The removal of a fully migrated IUCD from the bladder is typically performed during cystoscopy, often without difficulty if detected early, as in our case. In cases involving a calcified IUCD, lithotripsy may be necessary before removal. In more complex situations, such as when an IUCD has migrated into the bladder and ascended into the ureter, a cystotomy or laparotomy might be required. Additionally, some herbal remedies, like the Persian herbal recipe, are sometimes used to aid in stone ejection or dissolution without surgery. For vesicouterine fistulas, open or laparoscopic surgery [10] remains the preferred treatment to separately close the bladder and uterine openings of the fistula, with or without preserving the uterus.
Conclusion
As IUCDs are long acting, follow up by trained personnel to feel and locate IUCD thread at least every 6 months must be mandatory to avoid complications of uterine perforation n migration to adjacent viscera, and if misplaced IUCD found in bladder wall can be removed by just 0.5 cm incision.
- Ortiz ME, Croxatto HB (2007) Copper-t intrauterine device and levonorgestrel intrauterine system: Biological bases of their mechanism of action. Contraception. 75: S16-S30.
- Callahan RL, Brunie A, Mackenzie AC, Wayack-Pambè M, Guiella G, Kibira SP, et al. (2019) Potential user interest in new long-acting contraceptives: Results from a mixed methods study in burkina faso and uganda. PLoS One. 14: e0217333.
- Varela C, Siña E, Astorga AR, Lazo D, Ortiz J, Schoijet IM, et al. The walking iuds:" The gynecologists nightmare.
- Kallat A, Ibrahimi A, Fahsi O, El Sayegh H, Iken A, Benslimane L, et al. (2017) Le dispositif intra-utérin: À propos d’une complication rare et revue de la littérature. The Pan African Medical Journal. 27: 193.
- Paré A, Ouattara A, Yé D, Kabré B, Bako A, Abubakar B, et al. (2020) Management of intrauterine device migrated into the bladder: A case report and literature review. Case Reports in Urology. 2020 8850087.
- Grimaldi L, De Giorgio F, Andreotta P, D'Alessio MC, Piscicelli C, Pascali VL (2005) Medicolegal aspects of an unusual uterine perforation with multiload-cu 375r. Am J Forensic Med Pathol. 26: 365-6.
- Goyal S, Goyal S (2016) Displaced intrauterine device: A retrospective study. JMR. 2: 41-3.
- Ozgur B, Doluoglu O, Sarici H, Sunay M, Karagoz M, Eroglu M (2014) S277: Intrauterine device migration to two different localizations resulting in bladder stone and carrying the risk of vesicovaginal fistula. European Urology Supplements. 7: e1591.
- Vahdat M, Gorginzadeh M, Mousavi AS, Afshari E, Ghaed MA (2019) Cystoscopic removal of a migrated intrauterine device to the bladder; a case report. Contraception and Reproductive Medicine. 4: 1-4.
- Zhang NN, Zuo N, Sun TS, Yang Q (2020) An effective method combining various endoscopes in the treatment of intravesical migrated intrauterine device. Journal of Minimally Invasive Gynecology. 27: 582.


Figures at a glance