Aggressive Angiomyxoma of the Perineum
Received Date: August 07, 2024 Accepted Date: September 07, 2024 Published Date: September 10, 2024
doi: 10.17303/jwhg.2024.11.201
Citation: Ana Victoria Martin Corral, Lourdes Galan Raposo, Jose Santos Salas Vailen, Enrique Gonzalez-Diaz (2024) Aggressive Angiomyxoma of the Perineum. J Womens Health Gyn 11: 1-8
Abstract
A 50-year-old woman presented with a large mass on her right ischioanal fossa. After surgical removal, a diagnosis was made of aggressive angiomyxoma. These tumors are exceedingly rare, and hard to diagnose as they can be mistaken for other perineal entities, and the locally recurrences are frequent.
Keywords: Aggressive Angiomyxoma; Perineum; Right Ischioanal Fossa; Mesenchymal Tumors; Bartholin’s Cysts
Introduction
Angiomyxomas are rare mesenchymal tumors that usually appear in women in their 4th or 5th decade of life. Their growth is slow and usually painless, with unclear edges, and they are often confused with other entities such as perineal abscesses or Bartholin’s cysts. In order to properly identify them, imaging studies will need to be done. It has a characteristic appearance in both MRI and CT scans, due to a concentration of fusiform cells which has been described as a “swirl sign” or “swirled appearance”. However, its definite diagnosis will only be made by a histopathological study.
Its treatment poses a challenge due to a tendency to recur in the following months and even years, but wide consensus points at excisional surgery as the better treatment option. Long-term follow-up is recommended, with reported recurrence rates varying between 10% to 80%.
In the hopes of spreading awareness about this uncommon entity, we report the case of a 50-year-old woman with a growth on her right ischioanal fossa, which extended toward the perineum, and which turned out to be an aggressive angiomyxoma of the perineum.
Case Presentation
A 50-year-old woman presented with a complaint of pain during urination and vulvar pruritus for the past six months. The patient had a history of one vaginal delivery and an abdominal hysterectomy due to fibroids some years before.
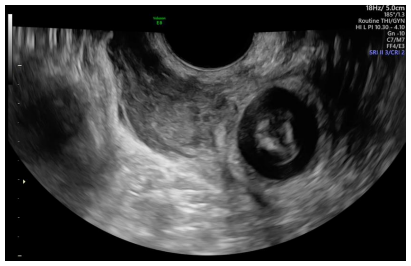
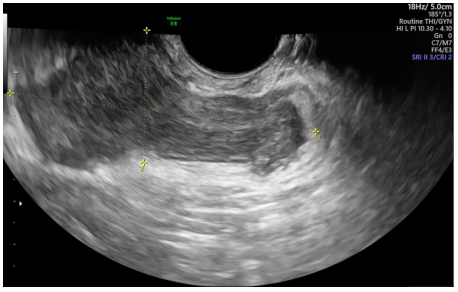
Upon examination, asymmetry of the right gluteus maximus could be noted, as well as a mass of soft consistency and unclear limits. A pelvic ultrasound was performed, reporting a low echogenicity mass with a surrounding pseudocapsule measuring 70x37 mm, beginning at the level of the anal canal in close contact with the external anal sphincter and going up the perineum and over the levator ani muscle, reaching the right paraurethral region. (Figures 1-2) 3D ultrasound showed how the mass displaced the puborrectal component of the levator ani muscle (Figure 3).
A pelvic MRI was performed, which described a cystic mass with heterogeneous intensity (seemingly mucous) measuring 91x61x26mm on the right hemipelvis. It confirmed that the mass spread from the perianal area of the perineum towards the right retropubic space (and right paraurethral space), and it lay over the levator ani muscle. It also lightly displaced the vagina and rectum towards the left.
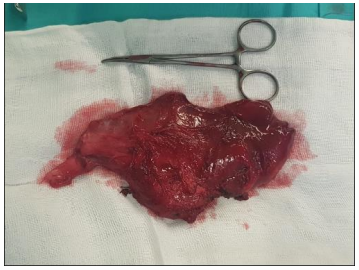
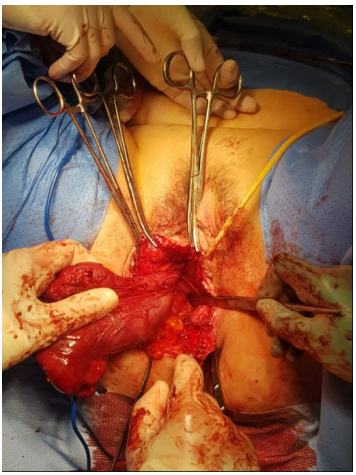
The patient was scheduled for surgical removal of the mass. With the patient in the lithotomy position, a surgical incision was made over the old scar of an episiotomy. A great tumour mass, encapsulated, an of soft consistency was located in the right ischioanal fossa, invading the right paravaginal and paraurethral spaces. It touched on and displaced the levator ani muscle. Resection of the mass was performed, managing to remove it in its entirety without rupturing it (Figure 4-5). During the resection of the mass from the anal sphincter, a lesion was made, which was subsequently repaired using 2/0 simple interrupted sutures. The surgical wound was closed using 0/0 thread and a Blake drain was left.
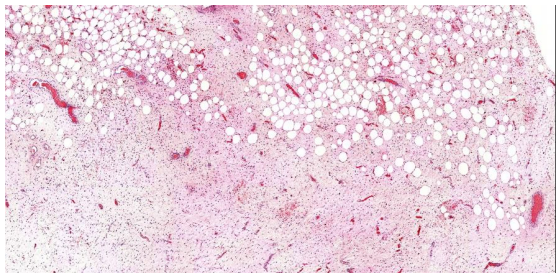
The histopathological report described an apparently delimited tumor formation measuring 10 x 8.5 x 3.5 cm in its maximum axis, with adipose tissue areas and a lobed pattern. The tumor was made up of spindle-shaped or stellate-shaped cells separated by an abundant myxomatous-looking stroma. The pathologist did not identify mitotic activity or cytological atypia. At the stromal level, abundant medium-sized vascular structures with slightly hyalinized walls were identified. Abundant trapped nerve structures were identified within the tumor. Adipose tissue was identified at a peripheral level, observing imprecise tumor limits, reaching the surgical edges of resection at some points (Figure 6). Immunohistochemical staining showed positive levels for estrogen and progesterone receptors and focally for CD34, while tumour cells were negative for S100 and KI67.
The histopathologic report diagnosed an aggressive angiomyxoma. Adjuvant treatments were ruled out and she was scheduled for close follow-up every 6 months (with MRI and ultrasound). As of three years later, no evidence of recurrence has been found.
Discussion
Aggressive angiomyxoma is a locally invasive benign mesenchimal tumour that can sometimes appear in the perineal or vulvar region. It is made up of spindle or stellate cells within a hypocellular myxoid tissue. It mostly appears in premenopausal women. It is a very rare entitity, with fewer than 50 cases found in the literature in the last decade.
It rarely methastasizes, with only 3 such cases reported in the literature [1]. It is mostly treated by local surgical excision. We also found one case that was treated with CT-guided percutaneous chemical ablation, although residual disease is described after the procedure [2].
Its main treatment challenge is not only achieving a complete excision, but its tendency to recur, even many years of the initial diagnosis and excision. Some groups have also tried giving GnRH-analogues either as neoadyuvant treatment (to shrink the tumour before surgical excision) or as maintenance treatment after the surgery. While there is no sufficient evidence regarding the use GnRH-analogues, some aggressive angiomyxomas express progesterone and/or estrogen receptors. And indeed, it has been shown in the literature that some of these tumours grow rapidly during pregnancy, which leads us to conclude that a hormonal influence could be responsible [3].
It would follow that for those angiomyxomas that showed progesterone and/or estrogen receptors, GnRH-analogues could be used as adjuvant treatment, at least in menopausal women (who account for a majority of the cases of angiomyxoma).
The adverse effects of their use such as headaches, hot flashes or osteoporosis could discourage premenopausal patients from using them chronically.
Aggressive angiomyxoma of the perineum and vulva often presents as a growing mass, without any other concomitant symptoms (although in rare cases it can cause painful urination or pruritus). It can also mask as a number of other clinical entities, most notably a Batholin’s cyst, an inguinal hernia or a lipoma [4].
Upon reviewing the literature, we found that this tumour is a rare entity in Europe and North America, with most cases stemming from Asia, especially those of bigger sizes [5,6].
Long-term follow-up is not standardized, though most cases suggest a 6-month or 1-year visit. It remains unclear whether follow-up MRIs are needed, since most patients who have a recurrence will consult with their medical providers immediately [7]. We would suggest a combined approach, alternating MRIs (which are costlier and usually have more scheduling conflicts) with transvaginal ultrasounds performed in clinic, ideally every 6 months [8].
Aggressive angiomyxoma poses a treatment challenge due to the inadequacy of using either chemotherapy or radiation therapy, given its low mitotic index. The mitotic index is the ratio between the number of cells in a population undergoing mitosis to the total number of cells in said population. An elevated mitotic index indicates more cells are dividing while a low one indicates that cells are diving slowly, and are more resistant to radiation and chemotherapy induced damages.
It is thus mostly treated with surgical excision but there is no consensus as to the surgical margins, since it is normally surrounded by similar connective tissue. These tumours usually lack a capsule and present grossly unidentifiable limits, making it hard for the surgeon to remove them completely. While they normally displace surrounding structures such as the vagina and rectum, as shown in our case, there are cases in the literature where they infiltrate surrounding structures [9].
Conclusion
Aggressive angiomyxoma of the perineum is a rare entity but it should always be in the differential diagnosis for a growing perineal mass. Surgical excision is the most common treatment, and the recurrences are frequent.
Conflict of Interest
The authors have stated explicitly that there are no conflicts of interest in connection with this article.
- Goyal P, Agrawal D, Sehgal S, Ghosh S, Kumar A, Singh S (2014) Aggressive angiomyxoma in pregnancy. Rare Tumors. 6: 5362.
- Li L, Chuang H, He-Nan L, Dong-Yuan L, Qing-Hua L, et al. (2023) Aggressive angiomyxoma of the pelvis and abdominal wall: Dramatic response to chemical ablation therapy. Front Oncol. 13: 1154283.
- Xu H, Sun P, Xu R, Wang L, Shi Y (2020) Aggressive angiomyxoma in pregnancy: a case report and literature review. J Int Med Res. 48: 300060520936414.
- Kumar N, Goyal A, Manchanda S, Sharma R, Kumar A, Bansal VK (2020) Aggressive pelvic angiomyxoma and its mimics: can imaging be the guiding light? Br J Radiol. 93: 20200255.
- Sinha V, Dave KS, Bhansali RP, Arora RS (2014) Aggressive angiomyxoma of vulva which grew with pregnancy and attained a huge size rarely seen in literature. J Obstet Gynaecol India. 64: 90-1.
- Sengupta SK, Bhattacharyya SK, Saha SP, Roy H, Sarkar AN (2014) Recurrent aggressive angiomyxoma of the vulva - a rare presentation. J Clin Diagn Res. 8: OD01-2.
- Peterknecht E, Agerbak E, Mohamedahmed A, Stonelake S, Kulkarni K, et al. (2021) Aggressive angiomyxoma of the ischioanal fossa in a post-menopausal woman. Ann R Coll Surg Engl. 103: e59-64.
- Tripathi A, Sharma S, Kanvinde S (2022) The Incidental Aggressive Angiomyxoma of the Vulva: Looks can be Deceptive. Gynecol Minim Invasive Ther. 11: 253-5.
- Zhao CY, Su N, Jiang YX, Yang M (2018) Application of ultrasound in aggressive angiomyxoma: Eight case reports and review of literature. World J Clin Cases. 6: 811-9.


Figures at a glance