Spectrum of Placenta Accreta: Perspectives from Four Years of Clinical Research at Constantine University Hospital
Received Date: December 21, 2024 Accepted Date: January 21, 2025 Published Date: January 24, 2025
doi: 10.17303/jwhg.2025.12.102
Citation: LAHAMR Manar, BICHA Soulef, MEZAACHE Houda (2025) Spectrum of Placenta Accreta: Perspectives from Four Years of Clinical Research at Constantine University Hospital. J Womens Health Gyn 12: 1-10
Abstract
In a few decades, the incidence of placenta accreta has increased considerably (approximately 1/1205 to 1/533 births). This increase is correlated with the increase in the cesarean section rate over the last 30 years.
The main objective: Identification of the frequency and factors of placenta accreta, as well as the results of management.
Materials and methods: Our prospective study is an inventory of the management of placenta accreta conducted at the level of the gynecology and obstetrics department of the Constantine University Hospital.
Results: Between January 1, 2015 and December 31, 2018, fifty-two cases of placenta accreta were recorded. The history of cesarean section is the main risk factor found in 96.2%, this risk is increased by the association with the low inserted placenta. The analysis of placenta accreta and the risk factors involved in their occurrence has allowed the development of a series of recommendations which aim to raise obstetricians' awareness of the search for signs of accretization in the presence of risk factors and to send these patients in structures adapted to the management of placenta accreta at an early gestational age, in order to schedule the birth between 34 weeks and 36 weeks.
Conclusion: We sought to calculate the frequency, identify the risk factors and evaluate our practices regarding the diagnosis and management of our patients with placenta accreta with the morbidity linked to each therapeutic attitude.
Keywords: Placenta Accreta; Cesarean; Gynecology and Obstetrics; Anatomopathological; Cataclysmic Hemorrhages
Introduction
In a few decades, the incidence of placenta accreta has increased considerably (approximately 1/1205 to 1/533 births). This is correlated with the increase in the cesarean section rate over the last 30 years. Faced with this resurgence and the fact that we were faced with its management in difficult situations, the diagnosis was often made intraoperatively during cataclysmic hemorrhages secondary to forced deliveries, or out of fear we proceeded with copious amounts of placenta with spectacular percritizations, the addition at the beginning was expensive in terms of maternal morbidity and mortality, since then we began our research into what was being done in the Maghreb and Africa, due to the fact that taking in charge in developed countries relied on remarkable human and material resources of expertise which we did not have, namely referent sonographers, MRI and technical platform for embolization. A roadmap was developed in order to optimize the management of PAS, identify the risk factors, optimize the antenatal DG by ultrasound and reinforce it if available by MRI, organize a technical platform with human skills surgery and anesthesia-resuscitation.
Materials and Methods
This work is a prospective study conducted at the level of the gynecology and obstetrics department of the Constantine University Hospital, between January 1, 2015 and December 31, 2018.
Our study population targeted all parturients who have at least one of the following risk factors: − Scarred uterus: cesarean section, curettage, operative hysteroscopy - Low placenta inserted, - Low placenta inserted on scarred uterus; - High maternal age; -Obesity. We included all cases of placenta accreta detected by pathological analysis on hystercomia specimens and cases suspected ultrasoundally with absence of placental abruption for conservative treatment. Maternal and fetal data were collected from obstetric and pediatric records. Data analysis was performed using SPSS software (SPSS for Mac, version 23.0, 2015, Chicago, IL).
Results
Between January 1, 2015 and December 31, 2018, there were 43,286 deliveries recorded at the gynecology and obstetrics department of Constantine University Hospital, including 20,757 by cesarean section performed at a gestational age greater than or equal to 22 weeks of amenorrhea (SA). ).
During the four years of the study we included 52 cases of placenta accreta. Our incidence of 1/833. These were 50 single-fetal pregnancies, two twin pregnancies (including one mono-chorionic bi-amniotic and one bi-chorionic bi-amniotic), two pregnancies with previa fibroids, and one death in utero on pregnancy of 33 weeks, the average is 13 cases per year with an average gestation of 4.25, of which 65.4% are multiparous. All our patients presented at least one of the risk factors described. The average number of cesarean sections is 1.94.
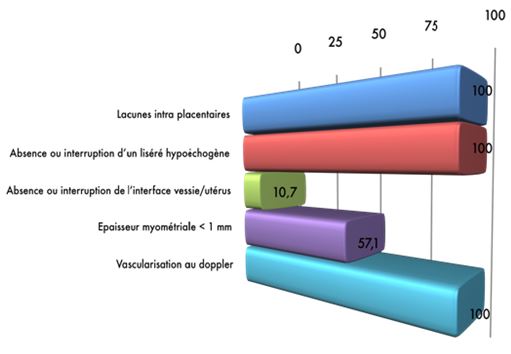
The distribution according to the number of cesareans shows that 36.5% (n19) have bi-scarred uteri, 32.7% (n=17) are single-scarred, 19.2% (n=10) are tri-scarred, 5.8% (n=3) are quadricereals and only 1 case of quinte scarred uterus which represents 1.9%, and two cases. 57.7% of patients are over 35 years old (n=30). The antenatal screening strategy (DAN) was essentially based on Doppler ultrasound used in 100% of cases, positive in 53.8% (n=28), for the rest the placenta accreta is diagnosed perpartum, with a rate of false negatives of 46.2% and placental MRI as second line in six cases of suspected placenta accreta, i.e. 11.5% of the overall population with a false negative rate of 50%. 86.5% of cases (n=45) it is an anterior placenta and in 13.5% of cases (n=7) a posterior placenta, including 90.4% low inserted repratis as follows Type 4 covering: 55.5% Type3 semi covering: 31.1% Type 2: 2.2% Non-low inserted: 11.1%; In the group of low inserted placentas 95.7% (n=45) occur on scarred uteri. In the group of non-lowly inserted placentas, all cases (n=5) occurred in a scarred uterus; for ultrasound signs were present in 53.8% of patients (n=28); distributed as follows (Figure 1).
All parturients in the study gave birth by cesarean section for the following obstetric indications: multi-scarred uterus, covering placenta. With an average term is 35 weeks ±6 days, with extremes ranging from 25 weeks to 42 weeks; of which 51.9% of births are at term (n=27) and 48.1% preterm (n=25 ). Of which 57.7% of cesarean sections were planned (n=30) and 42.3% were carried out urgently (n=22), note that in 21.2% it was general anesthesia (n =11), in 7.7% a locoregional anesthesia (n=4) and in 67.3% of cases a conversion from a locoregional anesthesia (LRA) to one general anesthesia (n=35)
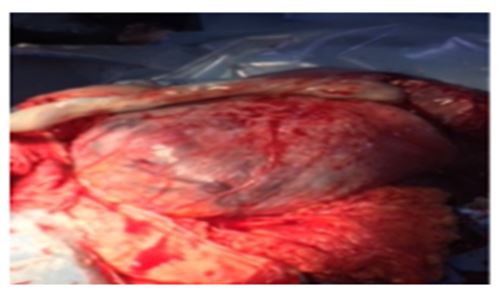
Among the clinical signs observed, we note that in 70.3% of cases (n=26) it is a neovascularization of the lower segment, and that in 29.7% of cases (n=11) it is a clear excessive placental invasion.
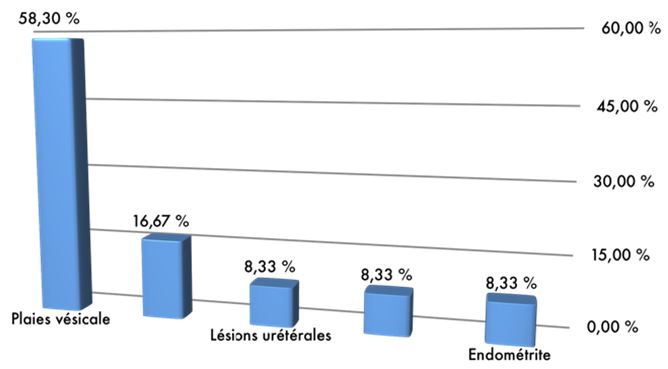
Caesarean section hysterectomy is the attitude most often performed in 86.5% of cases, (n=45) more marked in the case of DAN + and/or urgent cesarean section compared to 13.5% of cases (n=7) for conservative treatment. Group over 35 years old, radical treatment was carried out in 83.9% (n=26) and conservative treatment in 16.1% (n=5) with initial preservation of the fertility. Of all the patients transfused 69.2% (n=36) intraoperatively, we find 86.11% (n=31) of cases of hysterectomy and 13.88% (n=5) of cases of conservative treatment, with a overall complication rate of 23.1% (n=12) whatever the therapeutic attitude, it is twice as high in the case of conservative treatment compared to radical treatment (43% versus 20%), distributed as follows (Figure 2).
It is important to specify that during our study no maternal death from hemorrhage on placenta accreta was recorded.
The length of stay varies significantly depending on the therapeutic attitude, it is on average 5.5 days in the case of radical treatment versus 21.43 days in the case of conservative treatment (p=0.001). A pathological examination was carried out in 92% of cases, finding the following distribution: Placenta accreta: 61.5% (n=32) Placenta increta: 23.1% (n=12) Placenta percreta: 7.7% (n=4).
Discussion
The rate in our study is 1/833 included in the range reported in the literature. This variability can be explained in particular by the diversity of diagnostic criteria for placenta accreta between the different studies. Indeed, for certain authors, only cases diagnosed by the pathological examination of the placenta or the hysterectomy specimen were taken into account (pathological definition). For others when there was impossible or incomplete delivery with absence of cleavage (clinical definition).
Our patients were included taking into account both definitions
The age group between 33 to 35 years old; This is explained by the multiparity which is present in our cohort, as well as the constant desire for pregnancy, the refusal of tubal ligation in front of multi-scarred uteri for social reasons. In European studies this age limit is partly linked to late marriages. It would seem that multiparity is an element leading to the risk of placenta accreta and that maternal age is not a risk factor per se, it is rather the gynecological and obstetrical history of a woman over 35 years old, which would seem to be a risk factor for placenta accreta (multiparity, number of cesarean sections and history of curettage).
The risk of occurrence of placenta accreta increases with the number of previous cesarean sections [1-3]. We note that the history of a scarred uterus is indeed a predominant factor, however, it is not the only factor influencing the appearance of placenta accreta and that our Maghrib rates are higher compared to Western Europe made broader indications for cesarean section in our countries, by often insufficient monitoring of labor and the absence of the operating protocol for previous cesarean sections which should accompany the parturient at the time of delivery. 4.2% of cases the placenta was inserted low without uterine scar. This can be explained by the previous cesarean sections which could have been carried out before the formation of the lower segment which probably generated placental insertions next to the scars from high hysterotomies. Indeed, in our cohort, no inserted low-lying placenta is observed as the sole risk factor for placenta accreta; we find results which are similar to those of Miller et al [3], they consider that in the case of a low inserted placenta, the risk of myometrial invasion in the general population is 1/2500. Consequently we consider that low placental insertion alone does not constitute a force of placental invasion, therefore the low inserted placenta is an independent risk factor for placenta accreta according to our study and as demonstrated by Wu et al [2]. On the other hand, the association between scarred uterus and placenta previa is a high risk situation for placenta accreta, especially if the placenta is located on the uterine scar, well known since the work of Clark in 1985 [1,3]. In our series 95.74% of cases presented a low inserted placenta associated with a scarred uterus, this demonstrates the impact of the association of these two risk factors on the incidence of placenta accreta. The interest of a prenatal diagnosis is to schedule the delivery in a suitable department, level 3, it is essentially based on the echotomographic study, Doppler and MRI if necessary. For Attieh, placenta accreta must be suspected in any patient with placenta previa and a history of cesarean section or any other uterine surgery [4]. In our work, prenatal diagnosis was based on ultrasound examination as first intention, an MRI is requested if the ultrasound is not conclusive.
Placental gaps were present in 100% of placenta accreta diagnosed antenatally, these gaps were distributed between grades 1, 2 and 3 of the classification of Finberg et al [5]. This can be explained on the one hand by their aspects in Gruyère [6] easily recognizable on ultrasound and secondly because it constitutes the sign most sought after by our team. The absence of a hypo-echoic border between the placenta and the myometrium described in 1983 by Pasto et al [7] is found in 100% of diagnosed patients and 53% of our entire cohort. The hyperechoic line can be interrupted or bulging towards the bladder. It is a specific sign, but not very sensitive [5,6] our results can be explained by the low rate of placenta percreta 14.28% (n=4) found in our series, since this anomaly would be almost constant in the case of placenta percreta extended to the bladder [6,8] while for myometrial thickness < 1 mm is observed in 30.8%, in our examination Doppler vascularization is present in 53.8%; in the vast majority of cases, they do not improve the diagnostic relevance of 2D ultrasound for the detection of placenta accreta [1,7,8]. The low number of MRIs in our series does not allow us to evaluate our results.
In all cases, the patient must be informed of the risk of placenta accreta, and its possible consequences (severe hemorrhage during delivery, transfusions, hemostasis hysterectomy). We recommend a term of birth between 34 and 36 weeks in order to avoid the urgent nature of the delivery. With AG as type of anesthesia the clinical aspects suggestive of placenta accreta are the spectacular vascularization at the lower segment, particularly in relation to the accreted site and/or the clear visualization of placental invasion (Figure 3).
Indeed there is a clinically significant relationship between these signs and the degree of placental invasion especially for percreta (p=0.001), taking into account these clinical signs which allowed us intraoperatively to correct 75% of false negatives antenatal screening.
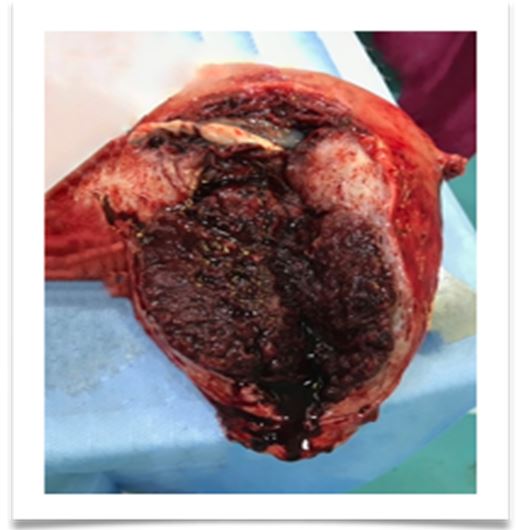
The so-called extirpative method was replaced in our work by a simple cautious attempt at delivery in the absence of clinical signs of accretization, because it is most often very hemorrhaging [10]. We have adopted in our work the 2 most standardized attitudes, namely a clearer trend for cesarean section-hysterectomy for hemostasis (Figure 4) compared to the expectant attitude.
The potential maternal benefits of early delivery must be weighed against the consequences of preterm birth and the associated increased risk of neonatal morbidity [11]. It was observed that 69% of parturients were transfused with CG, among them 11.5% polytransfused and 31% received a massive transfusion.
These results are undoubtedly linked to the high proportion of hysterectomies. Indeed, 69% of cesarean-hysterectomies were transfused.
Maternal Morbidity
For Radical Treatment: Bladder wounds: 58.3% (n=7) Ureteral lesions: 8.33% (n=1) Digestive wounds: 8.33% (n=1). For conservative treatment: Secondary hemorrhages: 16.67% (n=2); Endometritis: 8.33% (n=1).
The low rates observed in our series compared to similar studies can be explained by the obstetrical vocation of our service which annually counts a fairly large number of deliveries of around 13,000 births/year.
In our series we find among the 7 cases who initially retained their fertility, 43% of cases were secondarily complicated; either by hemorrhage in 28.57% of cases, or by endometritis in 14.28% of cases, this technique allowed us to avoid a hysterectomy in 57.15% of cases. These complications required a secondary hysterectomy. Monitoring of patients after conservative treatment is weekly until complete resorption of the placenta. It includes a clinical examination, a pelvic ultrasound and a biological assessment to look for an early infection (vaginal sample, CBC and CRP) [12].
During the period of our work, no maternal deaths from hemorrhage due to placenta accreta were recorded. This is explained by the availability of our team to deal with emergency situations in the event of serious postpartum hemorrhage in general and in particular the management of placenta accreta where we have remarkable experience, acquired from our daily practice of 'obstetrics. The length of stay is on average 5.5 days in the case of radical treatment compared to 21.43 days in the case of conservative treatment (P=0.001).
Therapeutic Attitude
In the current state of knowledge, forced delivery should be avoided and a cesarean-hysterectomy should be offered if the patient no longer desires pregnancy. We describe the cesarean-hysterectomy technique as it is practiced in our department with an operating time of 20 minutes Caesarean section-hysterectomy technique in case of placenta accretes.
1. Lower segment peritoneal abruption
2. Hysterotomy distant from the placental insertion
3. Fetal extraction
4. Perforate the subligamentous peritoneum of the teres and ovarian uterus at the same time or separately
5. Widen the opening with both fingers
6. Place a large ligation forceps on each side if taken from the round and utero-ovarian ligament in one step
7. Cut between the 2 pliers on each side (without tying, abandon the pliers on the ligatures)
8. Opening of the broad ligament to the fingers up to the paravagina at a distance from the ascending uterine artery
9. Ligation and division of the uterine artery and the cervicovaginal ones on each side, leaving the clamps on the ligatures
10. Begin the vesicouterine separation with the right index finger from the right vagina by tunneling the peritoneum towards the opposite side
11. Then raise the detachment of the peritoneum with the edge of the finger
vesico-vaginal from BOTTOM to UP until releasing the bladder (especially if percreta is suspected)
12. Opening the vagina with curved scissors
13. Removal of the uterus
14. Ligature quietly, finally to the wire by releasing the pliers
Please note that the average procedure time is 20 minutes. On the other hand, if the patient wishes to become pregnant, is young and nulli or primiparous, conservative treatment will be offered. We propose this Algorithm for the management of conservative treatment.
Strengths and Limitations of the Study
Limitations
The set of statistics targeted by our study lacks generalization criteria: the limited number of women, the heterogeneous epidemiological criteria. MRI is not always available without an embolization center.
Strengths
This is an obstetric problem whose frequency is increasing in Algeria, in the Maghreb country and even elsewhere in the world and which we have proposed a management protocol adapted to Algeria, namely for the treatment conservative or radical.
Conclusion
Since the recording of this pathology as a heavy daily burden for obstetricians, it was necessary to find specific and adapted care, especially in southern countries where the means are not always available both diagnostically and therapeutically, it was necessary to answer the two questions for ultrasound or MRI diagnosis and conservative or radical therapy, in conclusion of our work we proposed to optimize the ultrasound examination through continuing training and to favor radical treatment. Radical treatment (caesarean section-hysterectomy) in 86.5% of cases, conservative treatment (placental abandonment) in 13.5% of cases, this change of attitude was reflected following the high rates of maternal mortality at the service level during the years preceding the study (the overall MMR was 101.3 deaths per 100,000 live births). In our study we note an overall complication rate of 23.1% regardless of the therapeutic attitude is lower than those in the literature and we also note that the complication rate is twice as high in the case of conservative treatment compared to radical treatment (43% versus 20%). During this period, no maternal deaths due to placenta accreta hemorrhage were recorded, with a drop in overall MMR of 46.5%.
- Miller DA, JA Chollet, TM Goodwin (1997) Clinical risk factors for placenta previa-placenta accreta. Am J Obstet Gynecol, 177: 210-4.
- Wu S, M Kocherginsky, JU Hibbard (2005) Abnormal placentation: twenty-year analysis. Am J Obstet Gynecol, 192: 1458-61.
- Clark SL, PP Koonings, JP Phelan (1985) Placenta previa/accreta and prior cesarean section. Obstet Gynecol, 66: 89-92.
- Attieh E, et al. (1993) Placenta percreta and uterine rupture. Two cases report. 22: 649-52.
- Finberg HJ, JW Williams (1992) Placenta accreta: prospective sonographic diagnosis in patients with placenta previa and prior cesarean section. J Ultrasound Med, 11: 333-43.
- Comstock CH, et al. (2004) Sonographic detection of placenta accreta in the second and third trimesters of pregnancy. Am J Obstet Gynecol, 190: 1135-40.
- Pasto ME, et al. (1983) Ultrasonographic findings in placenta increta. J Ultrasound Med, 2: 155-9.
- Comstock CH (2005) Antenatal diagnosis of placenta accreta: a review. Ultrasound Obstet Gynecol, 26: 89-96.
- Placenta praevia: Evolution of ideas and therapies From Jacques Guillemeau to conservative cesarean section.
- Sentilhes L, et al. (2010) Placenta accreta: frequency, prenatal diagnosis, management, 2: 19-25.
- Eller AG, et al. (2009) Optimal management strategies for placenta accreta. BJOG, 116: 648-54.
- Kayem G, et al. (2007) Conservative versus radical management in cases of placenta accreta: a historical study. J Gynecol Obstet Biol Reprod (Paris), 36: 680-7.


Figures at a glance