An Unexplained Fever: A Rare Case of Tuberculous Endometritis
Received Date: January 18, 2025 Accepted Date: February 18, 2025 Published Date: February 21, 2025
doi:10.17303/jwhg.2025.12.104
Citation: Pr. Aboubekr F, Dr. Messaoud M, Dr. Bedjaoui H, Dr Tachema I, Dr. Senouci OS (2025) An Unexplained Fever: A Rare Case of Tuberculous Endometritis. J Womens Health Gyn 12: 1-7
Abstract
Female genital tuberculosis (FGT) is often latent and asymptomatic, with hematogenous spread from other sites being the primary mode of transmission. Its true incidence remains undetermined, as many cases go undiagnosed. While FGT can occur at any age, it is less common in postmenopausal women. Given its often subtle and persistent gynecological symptoms, endometrial tuberculosis should be considered in differential diagnoses, even in mild cases. The diagnostic process is complex, involving imaging techniques, biological tests, and histological analysis. This study presents a case of endometrial tuberculosis in a 56-year-old postmenopausal woman who sought consultation for unexplained fever and mild leukorrhea, highlighting the diagnostic challenges associated with genital tuberculosis.
Keywords: Genital Tuberculosis; Endometrial; Postmenopausal; Tuberculous Endometritis; Female Genital Tuberculosis
Introduction
Tuberculosis remains a public health issue in both developing and developed countries, despite efforts for its eradication, including routine vaccination at birth and standardized anti-bacillary treatment provided free of charge in specialized facilities.
According to the medical report on tuberculosis, 25% of the global population suffers from "latent tuberculosis", meaning they have been exposed to Mycobacterium tuberculosis but have not been infected by it and is not capable of transmitting it [1].
One type of extra pulmonary presentation of tuberculosis is the Female Genital Tuberculosis (FGT), which accounts 5% of all female pelvic infections and 10% of cases of pulmonary tuberculosis [2,3].
In its genital form, tuberculosis presents diagnostic challenges. The commonly encountered symptoms are nonspecific, which contributes to delays in treatment.
Genital tuberculosis can lead to irreversible damage to the female reproductive tract at progressive stages. Therefore, in the interest of prevention, early detection and management at the subclinical level are the only means to halt the damage and long-term sequelae to the female genital region [4].
Patients who are already infected with HIV or any other form of acquired or congenital immunodeficiency are at higher risk. Malnutrition, limited access to healthcare, and poverty are additional risk factors.
We report a case of endometrial tuberculosis that illustrates the diagnostic challenges of genital forms. This case serves to alert clinicians to consider the possibility of endometrial tuberculosis in a patient presenting with mild, common gynecological symptoms.
Case Report
A 56-year-old female patient, B.M., with a history of 3 pregnancies and 3 deliveries, has been postmenopausal for 11 years. Her medical history includes end- stage renal failure on dialysis (3 sessions per week), hypertension for 6 years under treatment, and asthma managed with corticosteroid therapy. She presents with unexplained fever for 2 months, with no identifiable infectious focus, leading to referral to our clinic for specialized consultation.
The patient’s history reveals no pelvic pain or metrorrhagia; however, vaginal discharge was reported. There is no history of tuberculosis exposure or signs of tuberculosis infection.
A speculum examination revealed a large cervix with some signs of infection, friable and bleeding upon contact, with the presence of small amounts of thick, sticky, non-malodorous white leukorrhea.
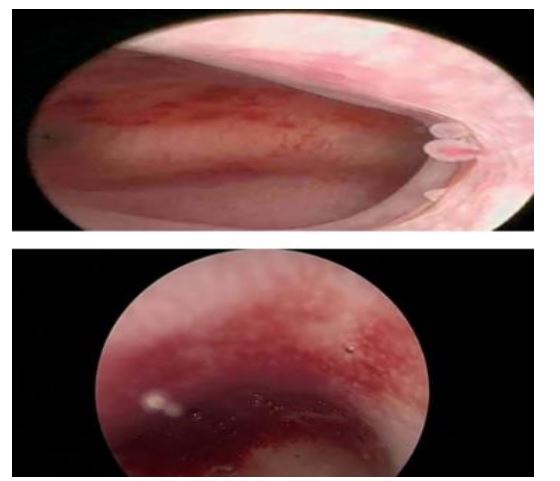
A pelvic ultrasound was performed, showing a subnormal-sized uterus with a small hypoechoic image measuring 10mm x 8mm, consistent with an intra-cavitary collection (Figure 1). The adnexa were unremarkable. Given this clinical presentation, a high genital tract infection was suspected.
The patient was placed on broad-spectrum antibiotic therapy, combined with an antipyretic treatment. Given the cervical appearance, the patient underwent a cervical smear, which indicated the presence of low-grade lesions. Consequently, a colposcopic examination with biopsy was performed, revealing low-grade cervical intraepithelial neoplasia (CIN1) associated with a condylomatous lesion of the exocervix.
A follow-up ultrasound was performed after the course of antibiotic therapy, showing the disappearance of the intracavitary image. Subsequently, a hysteroscopy was carried out, revealing a strawberry-like appearance of the endometrium (Figure 2), raising suspicion of endometritis. The cervico-isthmic canal appeared unremarkable, and the ostia were clearly visible.
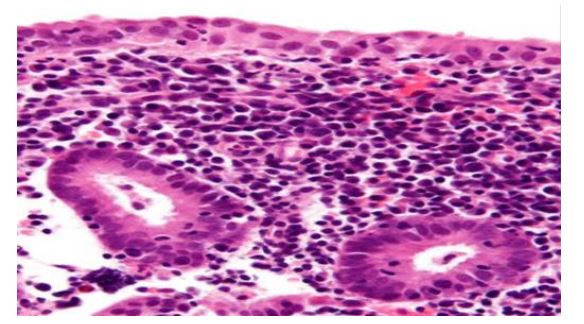
An endometrial biopsy was performed, and the histopathological study revealed an endometrial mucosa altered by a granulomatous inflammatory reaction composed of epithelioid and multinucleated giant cell granulomas of varying sizes and shapes, with no detectable caseous necrosis. This indicates granulomatous endometritis, with a possible tuberculous origin suggested despite the absence of caseous necrosis.
Since the histopathological examination did not identify a specific type of granulomatous infection, our therapeutic decision leaned toward a radical surgical approach, including total hysterectomy and bilateral salpingo-oophorectomy.
The postoperative course was favorable, with no complications. The patient was discharged after 72 hours of hospitalization.
The histopathological study of the surgical specimen reconfirmed granulomatous endometritis, with a tuberculous origin being the primary consideration. The patient was referred to an anti-tuberculosis center with a detailed medical report for specialized management, including anti-tuberculosis treatment.
Discussion
Tuberculosis remains a current global health concern, with nine million new cases and one and a half million deaths recorded annually. Extra pulmonary tuberculosis accounts for an increasingly significant proportion of new cases in developed countries, and this trend continues to rise.
The true incidence of genital tuberculosis is not well established, as many cases remain undiagnosed. Diagnosis is traditionally made in women of reproductive age. However, this condition can occur at any stage of life, including in the postmenopausal women and prepubertal girls, where intrauterine synechiae may lead to primary amenorrhea [6].
Exceptional cases of genital tuberculosis have been reported during menopause, most often secondary to other extra pulmonary sites. There is usually a long latency period between the initial focus, often pulmonary, and genital involvement [7].
Female genital tuberculosis is characterized by the high frequency of latent and asymptomatic forms. It is always secondary, resulting from either:
- Hematogenous dissemination from an initial tuberculous focus, with primary involvement of the fallopian tubes (100% of the cases), leading to a salpingitis-like presentation. The infection then progresses to other genital organs, affecting the endometrium (50% of the cases), ovaries (20%), cervix (5%), and vagina or vulva (8%).
- Lymphatic spread from pelvic lymph nodes.
Rare cases of direct inoculation through venereal transmission have also been reported by Weinstein [8].
Tuberculous endometritis in young women is almost always associated with tuberculous salpingitis, unlike in postmenopausal women, where endometritis is often isolated without tubal involvement [3].
This finding is supported by the histopathological examination of the surgical specimen from our patient, which revealed exclusive involvement of the endometrium, with intact fallopian tubes and no other genital involvement.
Genital tuberculosis is rare in postmenopausal women. The limited incidence of this disease in this age group is difficult to explain. Most authors believe that an atrophic endometrium provides an unfavorable environment for the growth of Mycobacterium [7,9].
Genital tuberculosis is often asymptomatic, and the disease may only manifest years after the primary infection. The most commonly reported reasons for consultation include infertility (44%), pelvic pain (25%), vaginal bleeding (18%), amenorrhea (5%), leukorrhea (4%), and postmenopausal metrorrhagia (2%). In rare cases, an abdominal mass, ascites, or a tubo-ovarian abscess may be observed. Our case confirms the paucity of clinical symptoms in genital tuberculosis. The patient presented only with leukorrhea and fever, without any history of abnormal bleeding, pain, or other symptoms. In this clinical context, several diagnoses can be considered, such as chronic non-tuberculous genital infections (Chlamydia, Gonococcus) or other infectious pathologies that may cause similar symptoms, which can be differentiated from bacterial or parasitic infections through specific microbiological tests. Given the patient's age and postmenopausal status, simple hyperplasia or endometrial cancer may also be considered, with endometrial biopsy being the only definitive diagnostic tool. Additionally, sarcoidosis, an inflammatory granulomatous disease, should not be overlooked.
Clinical examination is usually normal and rarely contributes to the diagnosis. This highlights the challenges associated with diagnosing tuberculosis in postmenopausal women. It is therefore important to consider the possibility of endometrial tuberculosis in patients with persistent leukorrhea that does not respond to well-conducted antibiotic treatment, particularly in tuberculosis-endemic areas. The diagnosis is challenging and requires imaging, biological, and histological investigations. In our patient, a pelvic ultrasound revealed intra-cavitary fluid retention, initially suggesting an upper genital tract infection. A diagnostic hysteroscopy was then performed, revealing an endometrial appearance consistent with endometritis (strawberry-like aspect).
The definitive diagnosis is established by identifying Mycobacterium tuberculosis, either through direct microscopic examination or by culturing pathological specimens. The analyzed material is typically obtained via endometrial biopsy curettage. However, in our case, the results were inconclusive, indicating granulomatous endometritis with a suspected tuberculous origin, despite the absence of caseous necrosis [13].
Histological examination of genital biopsies remains the key test to confirm the diagnosis, although caseous necrosis may be absent in true tuberculosis cases, as is the case in our patient. According to Taleb [12], a negative histological study does not rule out tuberculosis and should instead prompt repetition of the test. This led us to pursue radical surgical treatment.
The biological workup is of limited value, often showing accelerated sedimentation rate, lymphocytosis, and changes in gammaglobulins. Imaging techniques are not specific. Chest radiography may reveal parenchymal or pleural sequelae, and less frequently, evolving lesions [11]. In our patient, the biological tests were unremarkable, and the chest radiography was entirely normal. Most authors give special importance to hysterosalpingography, with two characteristic features of tuberculous origin: uterine synechiae and the vascular passage image, which produces the classic KIKA angiogram, observed in 30% and 15% of cases, respectively [12].
A recent technique, the GeneXpert test, is a rapid molecular test that detects the presence of *Mycobacterium tuberculosis* and can also identify resistance to rifampicin (one of the first-line drugs for tuberculosis treatment). Although this test is widely used for pulmonary tuberculosis, its role in the diagnosis of genital tuberculosis (including endometrial tuberculosis) is evolving, given its rapid results (approximately 2 hours), allowing for prompt initiation of treatment. This test also has good sensitivity and specificity for detecting *Mycobacterium tuberculosis* in samples, particularly endometrial or genital secretions specimens [15].
Therefore, the GeneXpert test has a role in the diagnosis of endometrial tuberculosis, but it should not be used as the sole diagnostic tool; it must always be combined with other methods.
The treatment is currently well-established and involves the daily administration of isoniazid and rifampicin for six months, combined with pyrazinamide and ethambutol during the first two months [6]. Clinical and Para-clinical monitoring is carried out regularly throughout the treatment.
Surgical treatment for genital tuberculosis is indicated in cases of persistence of adnexal masses despite medical treatment, particularly in the case of cold abscesses, recurrence of endometrial tuberculosis after one year of treatment, persistence of pelvic pain after 3 months of treatment or when it has not completely resolved after one year of treatment, persistent metrorrhagia after anatomical and clinical healing, and fistulas that do not heal [14].
Our patient underwent immediate surgical treatment since the histopathological examination was inconclusive. This was done to confirm the diagnosis and to preserve her genital health, even though menopause had occurred. Surgery was also performed to prevent potential systemic complications or to treat local abnormalities that could negatively impact her quality of life.
Although surgery is not always mandatory, it may be recommended for diagnostic, therapeutic, or complication management purposes. Each case must be evaluated individually, which was done by our medical team. The decision to proceed with a hysterectomy was made following a medical conference.
The patient was then referred to an anti-tuberculosis center for specialized management.
Conclusion
Tuberculosis remains common but rarely manifests as endometrial involvement. Young women from low socioeconomic backgrounds, who present with infertility, are most affected. However, it is important to consider tuberculosis in the presence of persistent pelvic symptoms, regardless of age, and to conduct the necessary diagnostic tests.
- Global Tuberculosis Report (2021) Geneva, Switzerland: World Health Organization.
- Namavar Jahromi B, Parsanezhad ME, Ghane-Shirazi R (2001) Female Genital Tuberculosis and Infertility. Int J Gynaecol Obstet. 75: 269-72.
- Sharma JB, Sharma E, Sharma S, Dharmendra S (2018) Female Genital Tuberculosis: Revisited. Indian J Med Res. 148: 0-83.
- Sharma JB, Sharma E, Sharma S, Dharmendra S (2021) Recent Advances in the Diagnosis and Management of Female Genital Tuberculosis. J Obstet Gynaecol India. 71: 476-87.
- Duggal S, Duggal N, Hans C, Mahajan RK (2009) Female Genital Tuberculosis and HIV Co-infection. Indian J Med Microbiol. 27: 361-3.
- Varma TR (1991) Genital Tuberculosis and Subsequent Fertility. IntJ Gynaecol Obstet. 35: 1-11.
- Maestre MA, Manzano CD, López RM (2004) Postmenopausal Endometrial Tuberculosis. Int J Gynaecol Obstet. 86: 405-6.
- Hammami B, Kammoun MF, Ghorbal H, et al. (2005) Female Genital Tuberculosis in Southern Tunisia (Review of 22 Cases). La Lettre du Gynécologie, 13.
- Gungorduk K, Ulker V, Sahbaz A, Ark C, Terkirdag AI (2007) Postmenopausal Tuberculosis Endometritis. Infect Dis Obstet Gynecol. 2007: 27028.
- Saygili U, Guclu S, Altunyurt S, Koyuncuoglu M, Onvural A (2002) Primary Endometrioid Adenocarcinoma with Coexisting Endometrial Tuberculosis: A Case Report. Journal of Reproductive Medicine. 47: 322-4.
- Gungorduk K, Ulker V, Sahbaz A, et al. (2007) Postmenopausal Tuberculosis Endometritis. Infect Dis Obstet Gynecol. 2007: 27028.
- Taleb AL, Bouchetara K, Boutteville C (1989) Female Genital Tuberculosis. Encycl Méd Chir (Paris-France), Gynécologie, 490. A10-7-1913.
- Elbahraoui H, Elmazghi A, Bouziane H, et al. (2012) Postmenopausal Tuberculous Endometritis Simulating Endometrial Cancer: Report of a Case. Pan Afr Med J. 11: 7.
- Ravelosoa E, Randrianantoanina F, Rakotosalama D, Andrianampanalinarivo R, Rakotomalala C, Rasolofondraibe A, et al. (2007) Female Genital Tuberculosis: A Study of 11 Cases in Antananarivo, Madagascar. Bull Soc Pathol Exot. 100: 30-1.
- https://www.sciencedirect.com/science/article/abs/pii/S0761842516307434


Figures at a glance